Researchers identify three sub-types of depression
According to the World Health Organization, nearly 300 million people worldwide suffer from depression and these rates are on the rise. Yet, doctors and scientists have a poor understanding of what causes this debilitating condition and for some who experience it, medicines don’t help.
Scientists from the Neural Computational Unit at the Okinawa Institute of Science and Technology Graduate University (OIST), in collaboration with their colleagues at Nara Institute of Science and Technology and clinicians at Hiroshima University, have for the first time identified three sub-types of depression. They found that one out of these sub-types seems to be untreatable by Selective Serotonin Reuptake Inhibitors (SSRIs), the most commonly prescribed medicines for the condition. The study was published in the journal Scientific Reports.
Serotonin is a neurotransmitter that influences our moods, interactions with other people, sleep patterns and memory. SSRIs are thought to take effect by boosting the levels of serotonin in the brain. However, these drugs do not have the same effect on everyone, and in some people, depression does not improve even after taking them. “It has always been speculated that different types of depression exist, and they influence the effectiveness of the drug. But there has been no consensus,” says Prof. Kenji Doya.
For the study, the scientists collected clinical, biological, and life history data from 134 individuals – half of whom were newly diagnosed with depression and the other half who had no depression diagnosis– using questionnaires and blood tests. Participants were asked about their sleep patterns, whether or not they had stressful issues, or other mental health conditions.
Researchers also scanned participants’ brains using magnetic resonance imaging (MRI) to map brain activity patterns in different regions. The technique they used allowed them to examine 78 regions covering the entire brain, to identify how its activities in different regions are correlated. “This is the first study to identify depression sub-types from life history and MRI data,” says Prof. Doya.
With over 3000 measurable features, including whether or not participants had experienced trauma, the scientists were faced with the dilemma of finding a way to analyze such a large data set accurately. “The major challenge in this study was to develop a statistical tool that could extract relevant information for clustering similar subjects together,” says Dr. Tomoki Tokuda, a statistician and the lead author of the study. He therefore designed a novel statistical method that would help detect multiple ways of data clustering and the features responsible for it. Using this method, the researchers identified a group of closely-placed data clusters, which consisted of measurable features essential for accessing mental health of an individual. Three out of the five data clusters were found to represent different sub-types of depression.
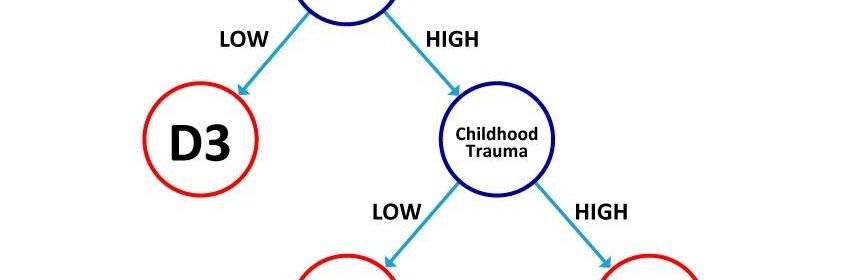
The three distinct sub-types of depression were characterized by two main factors: functional connectivity patterns synchronized between different regions of the brain and childhood trauma experience. They found that the brain’s functional connectivity in regions that involved the angular gyrus—a brain region associated with processing language and numbers, spatial cognition, attention, and other aspects of cognition—played a large role in determining whether SSRIs were effective in treating depression.
Patients with increased functional connectivity between the brain’s different regions who had also experienced childhood trauma had a sub-type of depression that is unresponsive to treatment by SSRIs drugs, the researchers found. On the other hand, the other two subtypes – where the participants’ brains did not show increased connectivity among its different regions or where participants had not experienced childhood trauma – tended to respond positively to treatments using SSRIs drugs.
Source: Read Full Article