Metabolic Syndrome Links With Increased Thyroid Cancer Incidence
The study covered in this summary was published in ResearchSquare.com as a preprint and has not yet been peer reviewed.
Key Takeaways
-
Metabolic syndrome, as well as its individual conditions, especially abdominal obesity, low levels of high-density lipoprotein (HDL) cholesterol, and elevated blood pressure, appear likely to contribute to the development of thyroid cancer.
-
The observations come from a large, nationwide, population-based, cohort study of more than 4.6 million people between 40 and 70 years old.
-
The findings showed that the risk of developing thyroid cancer was significantly associated with the presence of metabolic syndrome and its components.
-
Women with metabolic syndrome were 16% more likely to develop thyroid cancer compared with women without metabolic syndrome. Men with metabolic syndrome were 19% more likely to develop thyroid cancer compared with men without metabolic syndrome.
Why This Matters
-
Metabolic syndrome and its associated conditions are predictive of elevated thyroid cancer risk and may be useful for screening to help diagnose thyroid cancer at earlier stages.
-
Based on the findings, patients with metabolic syndrome as well as those with one or more metabolic syndrome conditions should undergo routine screening for thyroid cancer.
Study Design
-
The study used a South Korean population database maintained by the country’s public medical insurance system (National Health Insurance Service), which includes about 97% of the country’s population.
-
The analysis focused on 4,658,473 adults 40 to 70 years old who underwent two examinations through the insurance system during 2009–2011 with no history of cardiovascular disease or thyroid cancer and had complete data and follow-up through the end of 2017.
-
Based on their examinations during 2009–2011, 1,012,782 (22%) of the subjects had metabolic syndrome. The researchers based the metabolic syndrome diagnosis on published criteria.
-
The cohort included 47,325 people (1%) who were diagnosed with thyroid cancer during follow-up.
-
The investigators calculated the incidence of thyroid cancer per 10,000 person-years and the relative risk of thyroid cancer after adjusting for age and body mass index.
Key Results
-
The incidence of thyroid cancer per 10,000 person-years was 6.2 in men with metabolic syndrome and 5.2 in men without metabolic syndrome, and 21.3 in women with metabolic syndrome and 19.6 in women without metabolic syndrome. Both between-group differences were significant.
-
Each of the five metabolic syndrome conditions was significantly associated individually with the risk of developing thyroid cancer in women. In men, neither hyperglycemia nor hypertriglyceridemia was significantly associated with thyroid cancer risk, but the other three conditions showed significant associations with incident thyroid cancer.
-
In both sexes, abdominal obesity, elevated blood pressure, and low levels of HDL-cholesterol were linked with greater relative risks for developing thyroid cancer than the other two metabolic syndrome components.
-
Abdominal obesity had the highest relative risk for incident thyroid cancer in men, 1.34, followed by low HDL-cholesterol, and then elevated blood pressure. Among women, the relative risk for developing thyroid cancer linked with low HDL-cholesterol was 1.19, followed by elevated blood pressure, and then abdominal obesity.
-
Overall, women had higher rates of incident thyroid cancer than men, and incidence rates increased as the total number of metabolic syndrome components increased.
Limitations
-
Correlation does not equal causation, and it remains unclear whether the association of metabolic syndrome or its related conditions and the development of thyroid cancer is due to incidental overlap between two prevalent disorders or due to connected pathophysiologic mechanisms. Clarification of this uncertainty will require additional large-scale, multicenter studies.
-
The analysis excluded data that were not mathematizable, and it excluded subjective data, such as smoking status, alcohol consumption status, and physical activity. The study focused instead on concise analyses of basic demographic data, such as age and sex, anthropometric and laboratory measurements, and the status of metabolic syndrome and its components. This analytic strategy may have introduced selection bias.
-
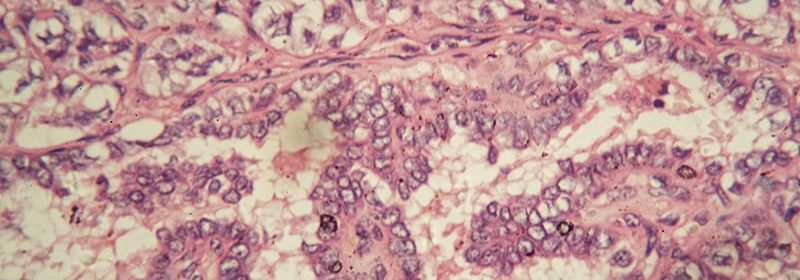
The study did not consider clinicopathologic data specific to thyroid cancer, which meant that the analyses did not account for histologic subtype, primary tumor size, extrathyroidal extension, lymph node or distant metastasis, nor the biological aggressiveness of the cancer.
-
The analyses did not account for the duration of metabolic syndrome or its conditions.
Disclosures
-
The study received no commercial funding and was supported by the Department of Surgery, Wonju Severance Christian Hospital, South Korea.
-
None of the authors had any disclosures.
This is a summary of a preprint research study, “The Importance of Screening for Thyroid Cancer in Patients with Metabolic Syndrome or its Components: A Nationwide Population-Based Cohort Study,” written by researchers at Yonsei University Wonju College of Medicine in South Korea on Research Square provided to you by Medscape. This study has not yet been peer reviewed. The full text of the study can be found on ResearchSquare.com.
Mitchel L. Zoler is a reporter with Medscape and MDedge based in the Philadelphia region. @mitchelzoler
For more diabetes and endocrinology news, follow us on Twitter and Facebook.
For more news, follow Medscape on Facebook, Twitter, Instagram, and YouTube.
Source: Read Full Article