Factors affecting SARS-CoV-2 transmission and outbreak control in densely populated areas
The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), which is the virus responsible for the coronavirus disease 2019 (COVID-19), originally emerged in December 2019 in Wuhan, China, and continues to spread worldwide. The transmission and deadly effects of COVID-19 have been significantly more considerable in densely populated regions such as Hong Kong and India.
Urban settings are more vulnerable to surges in COVID-19 as a result of close living conditions like dormitories, military camps, and apartment complexes. In an effort to reduce the spread of COVID-19 in these cities, several measures ranging from widespread lockdowns to targeted strategies in sub-populations to minimize disruption to society have been implemented.
A new study published in Scientific Reports seeks to identify the factors that lead to enhanced SARS-CoV-2 transmission, as well as the effects of control measures, in a dormitory in Singapore. This study included epidemiological, serological, and phylogenetic investigations that are supported by simulation models.
Background
In March 2020 in Singapore, scientists identified local community clusters with imported COVID-19 cases. These clusters included construction sites, commercial areas frequented by foreign workers, or foreign worker dormitories.
Specifically, the foreign worker dormitories had many common spaces, such as gyms and minimarts. These densely populated areas are assigned roughly 4.5 square meters per resident.
Any infectious disease has the potential to spread rapidly in these types of areas owing to the close constant contact between people. Therefore, it is important to understand the factors that could lead to a surge in COVID-19 cases so that potential future outbreak solutions and measures can be carefully planned.
About the study
In the current study, the scientists developed an individual-based model of a dormitory and augmented it with findings from epidemiological and serological investigations. The goal was to narrow down a set of factors that reproduced a similar outbreak trajectory in the dormitory.
To this end, the authors evaluated the efficacy of control measures present at the time and in alternative scenarios. Three scenarios were studied, which included:
- Baseline, which included only case isolation and roommates were required to quarantine
- Enhanced response and physical distance scenario, in which the deployment of teams expedited case isolation and enforcement of physical distancing measures
- Modified dormitory setting scenario in which there were reduced residents per room and en suite bathrooms were available. Shower and cooking facilities were also provided so that the individual quarantining stayed within the room.
Study results
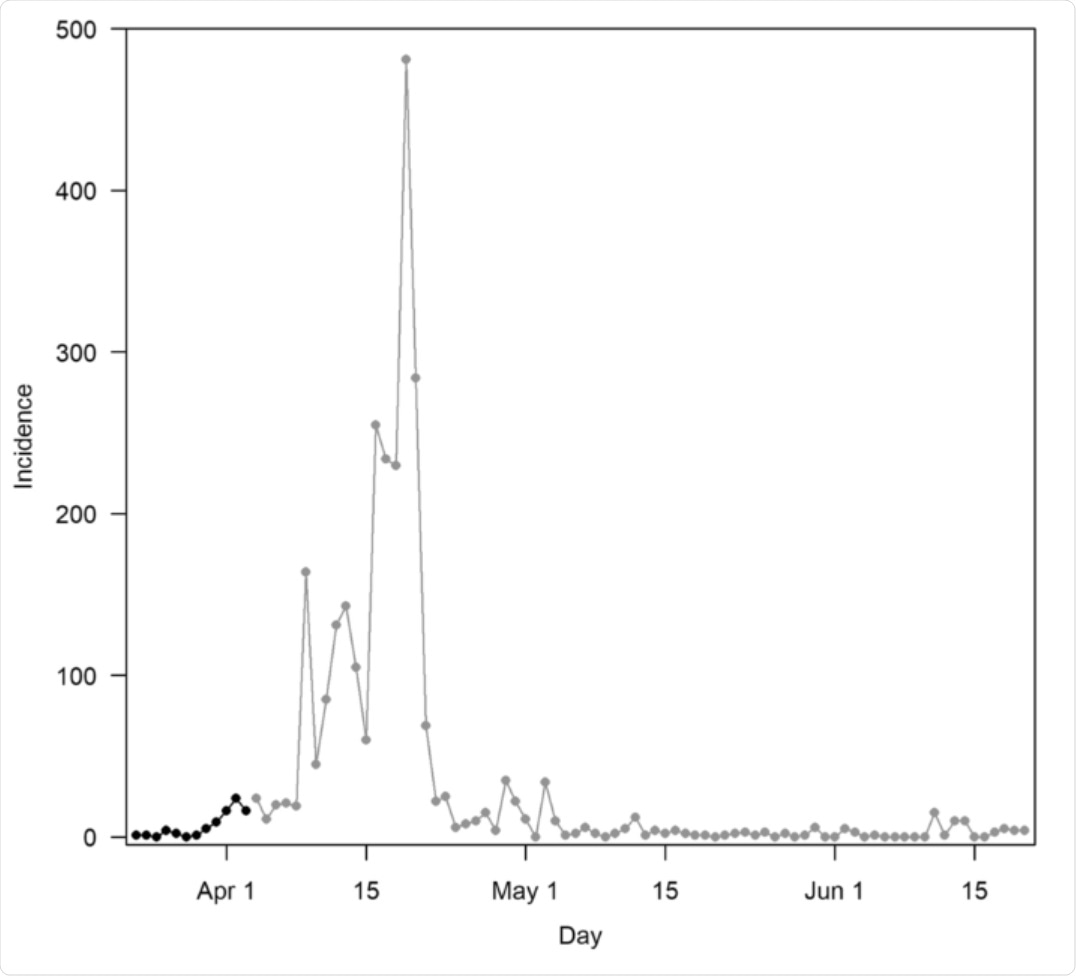
Between March 23 to June 20, 2020, 2,787 cases of COVID-19 were identified, none of whom had a travel history two weeks prior to the onset of symptoms. Post lockdown, or after April 6, 2020, cases declined.
A total of 7,367 workers participated in a seroprevalence survey, out of which 72% were seropositive and did not have a prior acute COVID-19 infection. Scientists sampled 10,000 parameter combinations and identified 13 cases that were needed for a sustained outbreak.
Based on these parameters, the current outbreak peaked at 511 infections on day 20 (76% attack rate). The peak was 905 in the baseline cases and 602 in the second group of participants. The scientists also conducted phylogenetic analyses and found that the genomes of the dormitory under study were similar and belonged to the pangolin lineage.
The scientists showed that, in the current scenario and at the time of the study, enhanced containment measures could reduce the attack rate by 22% as compared to the baseline. As a result, the peak cases could also be 40% lower. However, the outbreak duration was observed to be lengthened by 1-2 months.
About 71% of the infections were attributed to asymptomatic infections, whereas 57% of symptomatic cases did not require medical assistance. The model further estimated that each person had about 18 contacts outside the household, thus facilitating disease transmission.
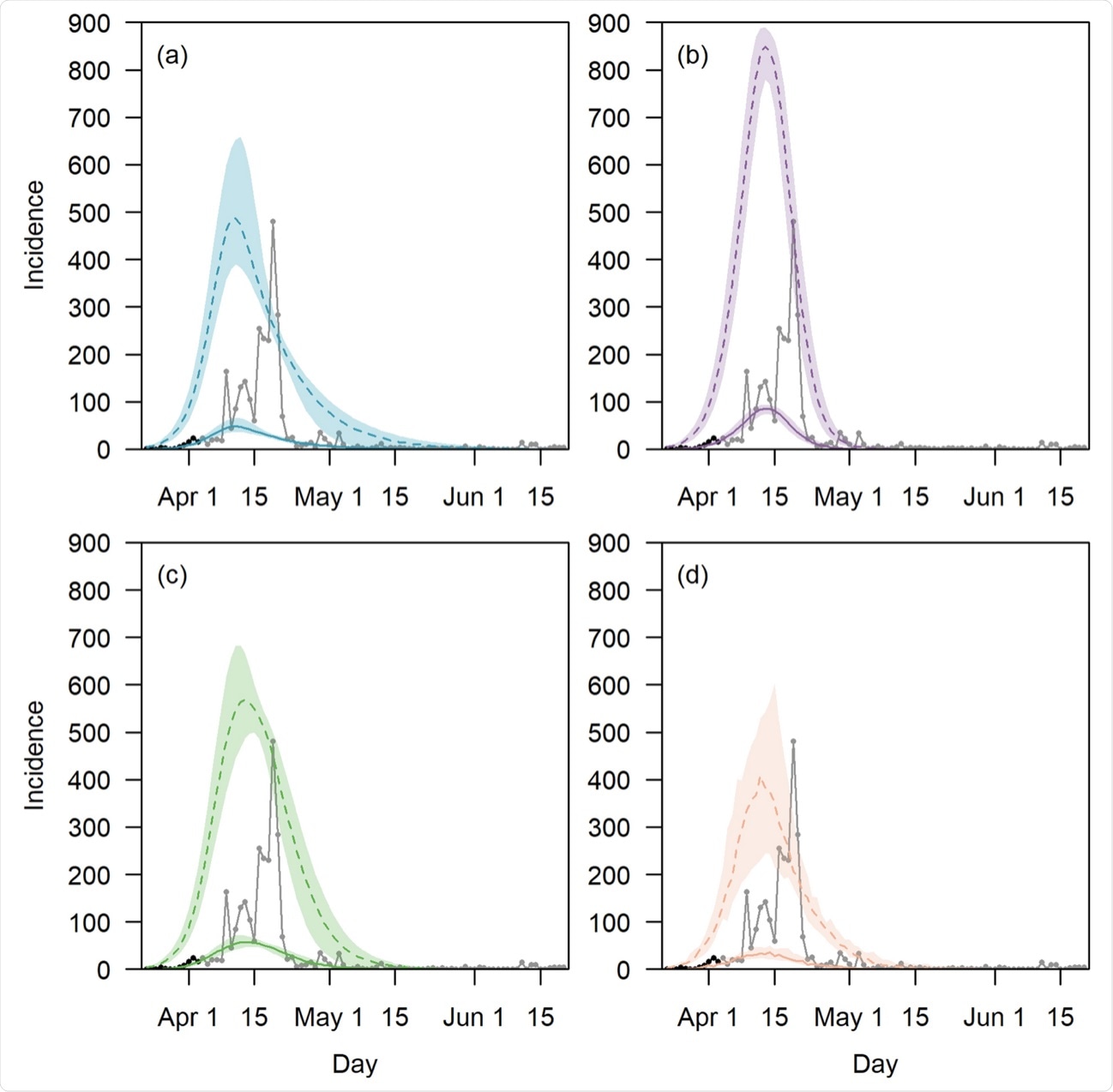
Taken together, these results point towards the need for increased living space, the availability of en suite washrooms, and lower occupancy per room. An increased living space could reduce the probability of infections by 10%, as shown by model simulations. The findings reported here could be carefully considered while designing high-density living areas in the future.
Limitations
Regular disinfection and housekeeping are common in dormitories; however, they were not included in the model. Furthermore, only dormitory cases in the pre-lockdown phase were used for model fitting.
The scientists also assumed that pre-symptomatic transmission could happen three days before symptoms appear and an individual is infectious up to fourteen days after the onset of symptoms. Although this is based on a number of studies, there is a considerable amount of uncertainty surrounding these bounds. Lastly, it would really help to model the specific profile of workers in dormitories and stratify the model by age, as infection in older individuals could result in more severe disease.
- Pung, R., Lin, B., Maurer-Stroh, S., et al. (2021). Factors influencing SARS-CoV-2 transmission and outbreak control measures in densely populated settings. Scientific Reports. 11. doi:10.1038/s41598-021-94463-3. https://www.nature.com/articles/s41598-021-94463-3.
Posted in: Medical Science News | Medical Research News | Disease/Infection News | Healthcare News
Tags: Coronavirus, Coronavirus Disease COVID-19, Disinfection, Efficacy, Respiratory, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Syndrome, Virus

Written by
Dr. Priyom Bose
Priyom holds a Ph.D. in Plant Biology and Biotechnology from the University of Madras, India. She is an active researcher and an experienced science writer. Priyom has also co-authored several original research articles that have been published in reputed peer-reviewed journals. She is also an avid reader and an amateur photographer.
Source: Read Full Article