Understanding how aggressive thyroid cancer evolves

Northwestern Medicine scientists have shed new light on how the deadliest form of thyroid cancer transforms from slow-growing to aggressive, according to research published in the Journal of Clinical Investigation.
Anaplastic thyroid cancer, one of the deadliest cancers worldwide, is a rare and highly aggressive tumor, according to the National Institutes of Health. Because of how aggressive the cancer is and how quickly it metastasizes, only 7% of patients with anaplastic thyroid cancer survive five years past diagnosis.
“Most cases of thyroid cancer are differentiated thyroid cancers, so patients don’t need aggressive treatments,” said Ruli Gao, Ph.D., assistant professor of Biochemistry and Molecular Genetics and senior author of the study. “Almost 99% of these patients survive to five years. A small fraction of those will transform into a dedifferentiated form of thyroid cancer, called anaplastic thyroid cancer.”
In the current study, investigators sought to understand how anaplastic thyroid cancer develops from indolent, or slow-growing, thyroid cancer.
“We wanted to figure out this complex intra-tumor evolution process by which cancer goes from indolent to highly lethal,” said Stephen Lai, MD, Ph.D., professor of Head and Neck Surgery at The University of Texas MD Anderson Cancer Center and co-corresponding author of the study.
To achieve this, the scientists performed high-throughput RNA sequencing and targeted DNA sequencing on anaplastic and papillary thyroid cancer tumors, as well as healthy thyroids. They then integrated their in-house data with large-scale bulk transcriptome and DNA datasets from the Cancer Genome Atlas (TCGA) database.
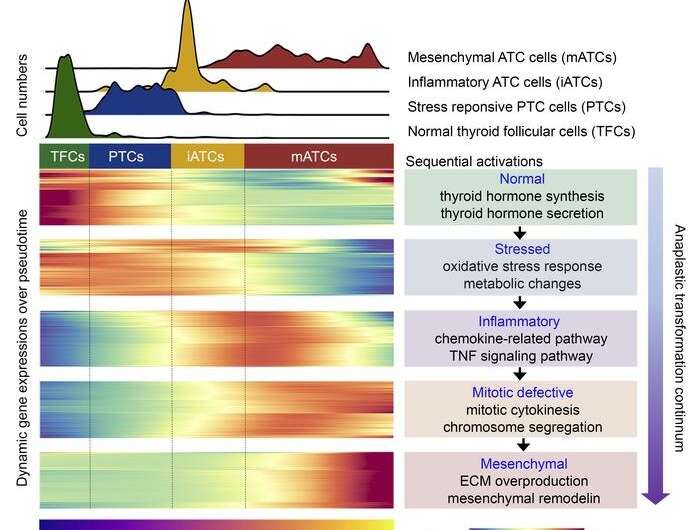
Utilizing a machine learning algorithm, investigators classified the molecular subtypes of the tumor cells using single-cell transcriptomics. They identified two key cell types associated with the progression of cancer: mesenchymal anaplastic thyroid cancer cells (mATCs) and inflammatory anaplastic thyroid cancer cells, or iATCs.
“Genetically, the iATC cells have diploid genomes, however their phenotypes are distinct. The mATC cells have aneuploid genomes that are common in solid tumors revealed by TCGA studies,” said Lina Lu, Ph.D., a postdoctoral fellow in the Gao Laboratory and first author of the study.
The new cell subtype identified, iATC, is the trigger for the transformation from indolent to aggressive thyroid cancer, Gao said. Once the cells transform from an inflammatory to a mesenchymal state, they begin to produce an excessive amount of collagen and begin to lose epithelial features.
“The findings could provide future therapeutic approaches for treating and preventing anaplastic thyroid cancers,” said Jennifer Wang, MD, Ph.D., assistant professor in the Department of Head and Neck Surgery at MD Anderson Cancer Center and co-first author of this study.
Moving forward, Gao said she and her collaborators hope to better understand the excessive production of collagen in mATCs and provide more insight to inform strategies to treat the cancer.
“Because anaplastic thyroid cancer is highly lethal and the patient dies very fast, we did not know a lot about the underlying molecular mechanisms,” said Gao, who is also a member of the Robert H. Lurie Comprehensive Cancer Center of Northwestern University. “This study really fills a gap in our knowledge. Now that we have this information, it’s like a sign physicians can use to see where a patient is at and to develop a strategy to treat them.”
More information:
Lina Lu et al, Anaplastic transformation in thyroid cancer revealed by single cell transcriptomics, Journal of Clinical Investigation (2023). DOI: 10.1172/JCI169653
Journal information:
Journal of Clinical Investigation
Source: Read Full Article