Study suggests causative pathway between gum disease and rheumatoid arthritis
Rheumatoid arthritis (RA), which causes painful swelling of the joints, is a form of autoimmune disease where otherwise healthy tissue in a patient’s joint gets mistaken for an intruder and is attacked by the immune system. Past observational studies have confirmed a correlation between patients with RA and higher levels of periodontal disease (gum disease).
Anti-citrullinated protein antibodies (ACPAs) are found in the blood of most patients with RA. They are correlated so tightly that ACPAs detected in the blood are the best early detection tool for future RA pathology as they can pre-date clinical diagnosis by several years. Gum disease is specifically more common in individuals with RA who also have ACPAs in their blood.
In a study led by Stanford University, researchers wanted to investigate whether these overlapping observations could be better connected.
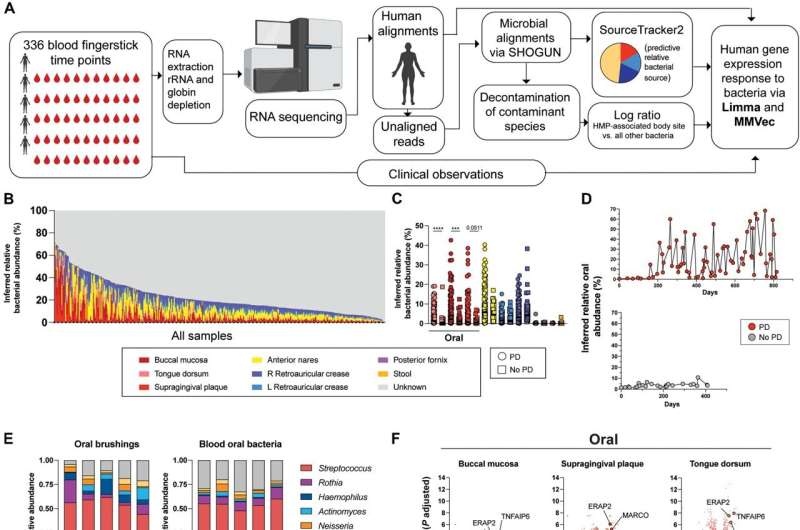
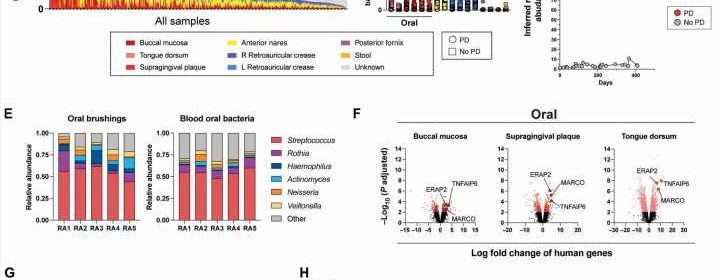
Researchers analyzed bacterial RNA in blood samples collected from a group of 5 RA patients with and without gum disease over weekly time points for a year. They identified RNA signatures within clusters of activated immune cells that correlated with both the presence of oral bacteria in the blood and with flares of arthritis in patients with both RA and periodontal disease.
The bacteria were found to be citrullinated (enzymatically altered), and this alteration provided the targets for the anti-citrullinated protein antibodies to attack, as well as increasing the number of antibodies responding. Researchers further found the bacteria to be already citrullinated in oral samples.
While this was a promising observation, it was still a correlation in the middle of previously known overlapping conditions. The researchers wanted to know whether the bacteria were causing the immune response, or if the RA was causing the response to the bacteria.
So, they took a more causational approach and attempted to directly trigger similar gene expression responses in vitro. Oral bacteria isolated from healthy individuals were pooled with blood from healthy individuals, and researchers looked for the presence of specific RNA compared to that of RA patients.
They detected robust expression of the specific RNA after six and 20 hours, illustrating that not only can oral bacteria induce systemic inflammatory response if they find their way into the blood, but that the response is not specific to patients with existing RA.
The researchers suggest that future studies are needed to determine whether improved oral care may provide therapeutic benefits in the management of RA.
The paper, “Oral mucosal breaks trigger anti-citrullinated bacterial and human protein antibody responses in rheumatoid arthritis,” is published in the journal Science Translational Medicine.
More information:
R. Camille Brewer et al, Oral mucosal breaks trigger anti-citrullinated bacterial and human protein antibody responses in rheumatoid arthritis, Science Translational Medicine (2023). DOI: 10.1126/scitranslmed.abq8476
Journal information:
Science Translational Medicine
Source: Read Full Article