Scientists Find Brain Signals of Chronic Pain
Researchers have for the first time recorded the brain’s firing patterns while a person is feeling chronic pain, paving the way for implanted devices to one day predict pain signals or even short-circuit them.
Using a pacemaker-like device surgically placed inside the brain, scientists recorded from four patients who had felt unremitting nerve pain for more than a year. The devices recorded several times a day for up to six months, offering clues for where chronic pain resides in the brain.
The study, published on Monday in the journal Nature Neuroscience, reported that the pain was associated with electrical fluctuations in the orbitofrontal cortex, an area involved in emotion regulation, self-evaluation and decision making. The research suggests that such patterns of brain activity could serve as biomarkers to guide diagnosis and treatment for millions of people with shooting or burning chronic pain linked to a damaged nervous system.
“The study really advances a whole generation of research that has shown that the functioning of the brain is really important to processing and perceiving pain,” said Dr. Ajay Wasan, a pain medicine specialist at the University of Pittsburgh School of Medicine, who wasn’t involved in the study.
About one in five American adults experience chronic pain, which is persistent or recurrent pain that lasts longer than three months. To measure pain, doctors typically rely on patients to rate their pain, using either a numerical scale or a visual one based on emojis. But self-reported pain measures are subjective and can vary throughout the day. And some patients, like children or people with disabilities, may struggle to accurately communicate or score their pain.
“There’s a big movement in the pain field to develop more objective markers of pain that can be used alongside self-reports,” said Kenneth Weber, a neuroscientist at Stanford University, who was not involved in the study. In addition to advancing our understanding of what neural mechanisms underlie the pain, Dr. Weber added, such markers can help validate the pain experienced by some patients that is not fully appreciated — or is even outright ignored — by their doctors.
Previous studies had typically scanned the brains of chronic pain patients to observe changes in blood flow in various regions, an indirect measure of brain activity. Such research is restricted to laboratory settings, however, and requires patients to visit a hospital or laboratory several times.
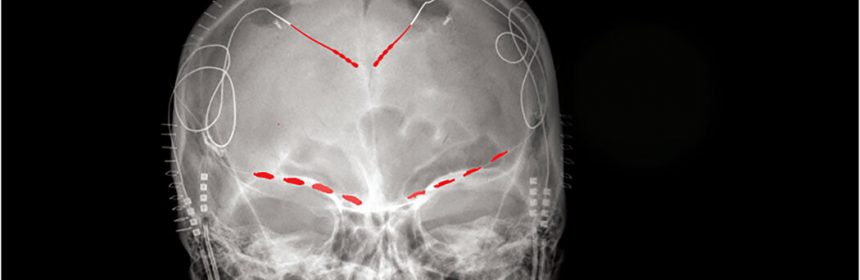
In the new study, Dr. Prasad Shirvalkar, a neurologist at the University of California, San Francisco, and his colleagues instead used electrodes to measure the collective firing pattern of thousands of neurons in the electrodes’ vicinity.
The researchers surgically implanted the recording devices into four people who had been living with pain for more than a year and had found no relief through medications. For three of the patients, the pain began after a stroke. The fourth had so-called phantom limb pain after losing a leg.
At least three times a day, patients would rate the pain they were feeling and then press a button that would spur their implants to record brain signals for 30 seconds. By following patients daily, at home and at work, “this is the first time ever chronic pain has been measured in the real world,” Dr. Shirvalkar said.
The researchers placed electrodes in two brain areas: the orbitofrontal cortex, which hasn’t been studied much in pain research, and the anterior cingulate cortex, a region involved in processing emotional cues. Many studies have suggested that the anterior cingulate cortex is important for perceiving both acute and chronic pain.
The scientists fed the data on the patients’ pain scores and the corresponding electrical signals into machine learning models, which could then predict high and low chronic pain states based on brain signals alone.
The researchers found that certain frequency fluctuations from the orbitofrontal cortex were the best predictors of chronic pain. Although that brain signature was common among patients, Dr. Shirvalkar said, each patient also showed unique brain activity. “Every patient actually had a different fingerprint for their pain,” he said.
Given these variations and just four study participants, Tor Wager, a neuroscientist at Dartmouth College who was not involved in the study, suggested caution in dubbing orbitofrontal cortex signatures as biomarkers just yet.
“We definitely want to corroborate this with other studies using other methodologies that can provide systematic coverage of the whole brain,” he said.
The study’s authors also noted that other brain regions may be involved. “We’re just getting started,” said Dr. Edward Chang, a neurosurgeon at the University of California, San Francisco. “This is just chapter one.”
The implants serve another purpose: deep brain stimulation. As part of a larger clinical trial to treat chronic pain, Dr. Shirvalkar and his colleagues are using mild electrical currents to stimulate the brain regions near the electrodes. In addition to the four patients in the study who are receiving this experimental therapy, the researchers aim to recruit two more people and eventually expand the study to 20 or 30 people. The researchers hope to relieve patients’ lingering pain by sending pulses through the electrodes to correct for any aberrant brain activity.
Source: Read Full Article