Q&A: A fourth of US health visits now delivered by non-physicians
The proportion of health care visits delivered by nurse practitioners and physician assistants in the US is increasing rapidly and now accounts for a quarter of all health care visits, according to a study published Sept. 14 in the BMJ.
The analysis, led by researchers from the Department of Health Care Policy in the Blavatnik Institute at Harvard Medical School, highlights the rising importance of this rapidly growing segment of the U.S. health care system.
The research is the first nationally representative study of the share of health care delivered by nurse practitioners and physician assistants, collectively known as advanced practice providers. It is also the first study to look at care delivered across different clinical conditions. The researchers analyzed 276 million visits from a nationally representative sample of Medicare insured patients.
Study co-authors Ateev Mehrotra, professor of health care policy at HMS, and Sadiq Patel, a former NIH postdoctoral fellow at HMS, spoke with HMNews about the increasingly important role these providers play in our health care system.
Harvard Medicine News: How did we get to the point where a quarter of all medical visits are conducted by nurse practitioners and physician assistants, not by physicians?
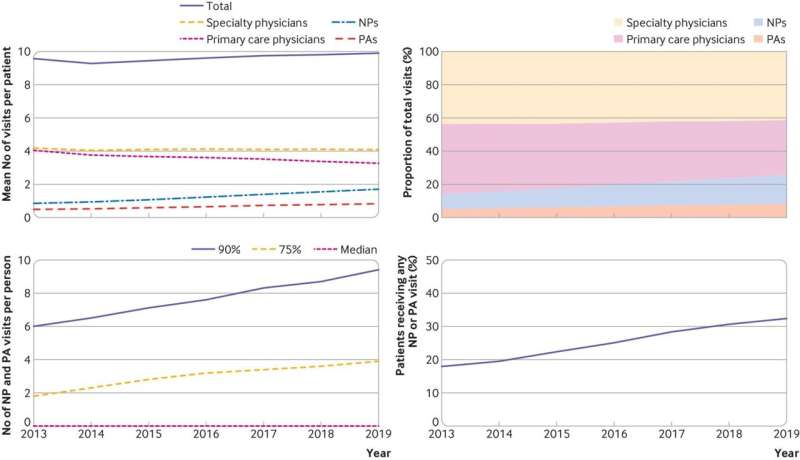
Mehrotra: The roles of nurse practitioners and physician assistants were created in the mid 1960s to address what were already identified at that time as physician shortages. We looked specifically at the years from 2013 to 2019, when the proportion of all traditional health care visits delivered by nurse practitioners and physician assistants increased from 14% to 25.6%.
That’s the average, but it varied across different conditions: 47% of respiratory infection visits and 31% of visits for anxiety disorders were conducted by nurse practitioners and physician assistants, but it was only 13% for eye disorders and 20% for hypertension.
HMNews: What’s driving this recent growth?
Mehrotra: The short answer is supply and demand. The U.S. has fewer physicians per capita than most of our peer nations. Who is going to provide that care? The number of nurse practitioners and physician assistants has grown more quickly than the number of physicians. And this trend will only continue as we move forward.
The U.S. Bureau of Labor Statistics estimates that between 2019 and 2031 the number of nurse practitioners in the U.S. will increase by 80% and the number of physician assistants by nearly 50%. In contrast, the growth rate for physicians over the next decade or so is estimated at less than 5%.
HMNews: Are there some patients who are more likely to see nurse practitioners or physician assistants than others?
Patel: Nurse practitioners and physician assistants are very widespread: Among all patients with at least one visit in 2019, 42% had one or more nurse practitioner or physician assistant visits. But there were some groups more likely to see nurse practitioners and physician assistants. The likelihood was greatest among patients who were lower income, rural residents, and people with disabilities.
That’s another reason it’s so important to get this right. We’ve known that these groups often have greater difficulty accessing care, and nurse practitioners and physician assistants are critical to providing this access.
HMNews: When people are sick, they usually think about ‘going to the doctor.’ Is this change worrying? Is there a difference in quality or cost between the care delivered by nurses and physician assistants versus the care delivered by physicians?
Mehrotra: First of all, it’s very important to emphasize that it’s not really a question of one or the other. Almost all these practitioners work in teams that include physicians, nurse practitioners, and physician assistants working together.
Most of the research agrees that all three professions can do a good job delivering care in most settings, especially primary care. And it turns out that there is not a significant difference in spending. But there are clinical conditions that might be better suited to one profession or another.
Patel: One of the things that we wanted to do with this study was to start looking at the specific types of care these allied professionals were most likely to deliver.
HMNews: What did you learn?
Patel: As Ateev mentioned, patients were less likely to see a nurse practitioner or a physician assistant for an eye disorder, and more likely to see them for a respiratory infection. That seems like a reasonable allocation of resources, given the relative complexity of the clinical conditions.
The high use of nurse practitioners and physician assistants for anxiety disorders is another interesting example. There simply aren’t enough psychiatrists to treat all the people who need care for mental health conditions. But the good news is that there are highly effective evidence-based treatments that can help a lot of people with depression and anxiety that do not require a physician to deliver.
Mehrotra: Hopefully one benefit that will follow from this research is that we will be able to identify the services that allied health professionals can deliver and provide the training and support services they need to take care of their patients, like proactively planning for remote supervision in more complex psychiatric services or specialist consults by telemedicine.
HMNews: Any predictions on how these changes will shape health care going forward?
Mehrotra: The increase in care delivery by nurse practitioners and physician assistants represents a massive change. We need more research on how to best structure teams of clinicians—nurse practitioners, physician assistants, and physicians—so that they can work together to provide the most effective care possible. If we are thoughtful about how we move forward as those changes continue to happen, that’s millions of opportunities to do it better. I hope we take advantage of that opportunity.
More information:
Sadiq Y Patel et al, Provision of evaluation and management visits by nurse practitioners and physician assistants in the USA from 2013 to 2019: cross-sectional time series study, BMJ (2023). DOI: 10.1136/bmj-2022-073933. www.bmj.com/content/382/bmj-2022-073933
Journal information:
British Medical Journal (BMJ)
Source: Read Full Article