How many babies die from genetic diseases because they’re not tested? Too many, researchers say

Genetic diseases kill more infants than anyone realizes.
That’s the central conclusion of a new study from the Rady Institute for Genomic Medicine in San Diego. The paper, published online Thursday, uses whole-genome genetic sequencing to examine the circumstances of 112 San Diego County babies who died from 2015 through 2020.
Researchers found evidence of “single locus” gene mutations in 46 babies that are linked to fatal conditions such as polycystic kidney disease, CHARGE syndrome and trisomy 21. Examining each child’s medical history and searching medical literature, they found that there were medical treatments available for 14 of the identified genetic diseases. In five cases, findings conclude that had timely diagnosis and treatment been available, “death might have been avoided.”
Dr. Euan Ashley, a personalized medicine specialist who directs the Clinical Genome Program at Stanford University, read the paper and said he agrees with the suggestion that earlier analysis could prevent death by helping start treatment sooner.
“Few deaths are more tragic than the death of a child,” Ashley said. “This study shows that a test, the basic (sequencing) element of which is now available for $200, is likely to have dramatic benefits if deployed early in the clinical course.”
The investigation also examined the death certificates completed for all 46 babies with disease-linked genetic mutations, finding that no genetic condition was noted as the root cause in 28. Because these conditions do not have their own category in national guidelines for categorizing causes of death, researchers created one, finding that 41 percent of deaths had a genetic cause.
It’s a significantly larger share than is visible in the most-recent accounting of infant mortality in the United States published by the National Vital Statistics System. In 2020, the report attributes 4,047 of the nation’s 19,578 deaths—21%—before age one to “congenital malformations, deformations and chromosomal abnormalities.”
Dr. Stephen Kingsmore, the Rady institute’s director, explained that the current classifications system for deaths masks the genetic origins.
“The way classification is done is sort of by organ system and hasn’t kept pace with our ability to decode genomes and to understand what’s going on at the DNA level,” Kingsmore said. “It reflects a 1940s or 1930s understanding of what causes death.”
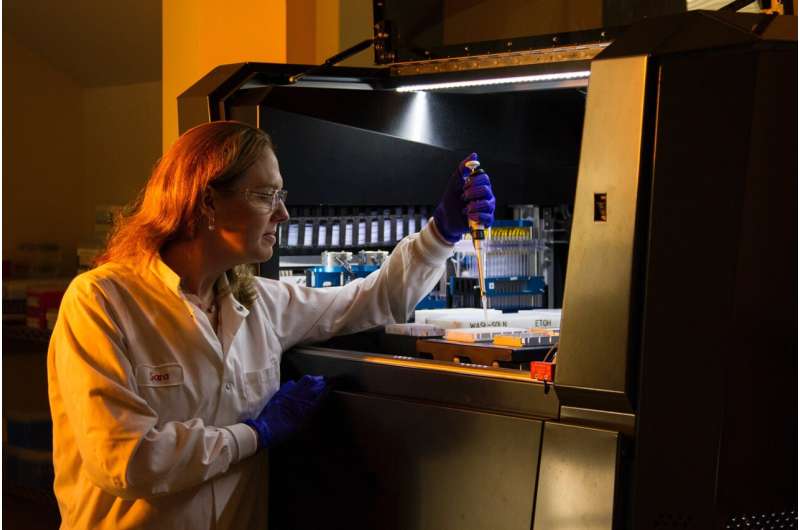
The physician and geneticist has pushed for better access to genetic analysis for newborns for years, now promoting BeginNGS, a screening system that uses dried blood samples collected from a newborn’s heel shortly after birth to search for about 400 rare genetic diseases that have proven treatments available.
These tests, he noted, cost hundreds rather than thousands of dollars, as is the case for whole-genome sequencing.
Thus far, though, health insurance companies are not required to pay for genetic testing of babies who might benefit. But that’s starting to change. Michigan, Minnesota and Louisiana have all enacted progressive coverage requirements for genetic sequencing.
“Michigan recognized that it was wrong, and they pay, I think, $6,000 for a genome when the baby could benefit,” Kingsmore said. “Minnesota went further, and they said ‘we’re going to cover all children, not just infants,’ and then Louisiana went one further still and they said ‘we’re going to mandate that the private payers also have to pay if they’re operating in Louisiana.'”
The California Legislature appropriated $3 million in the state budget so that Medi-Cal could begin paying for genetic testing statewide in 2022, but Kingsmore said that, so far, he is unaware of payment being approved for individual infants.
State Assemblyman Brian Maienschein first introduced a bill—AB-114—in 2021 that called for Medi-Cal funding, and a spokesperson in his Sacramento office said by email Wednesday that the benefit “went live as a covered Medi-Cal benefit on Jan. 1, 2022,” with the legislator’s office having “not been made aware of any patients or providers who have had trouble accessing this benefit.”
Ashley, the Stanford genetic specialist who recently broke Kingsmore’s Guiness World Record for the shortest genetic sequencing time, predicted in an email that insurance companies will eventually come around to the fact that early diagnosis often prevents long, expensive hospital stays.
“Any new technology takes some time to be adopted and, in general, payors want to find any reason not to pay,” Ashley said. “In this case, however, it is short-sighted because performing the test earlier would not only save lives but money too.”
2023 The San Diego Union-Tribune.
Distributed by Tribune Content Agency, LLC.
Source: Read Full Article