How Immunotherapy Might Be Used to Treat Heart Failure
A cutting-edge cancer treatment can also cure certain kinds of heart failure in mice, scientists reported on Wednesday.
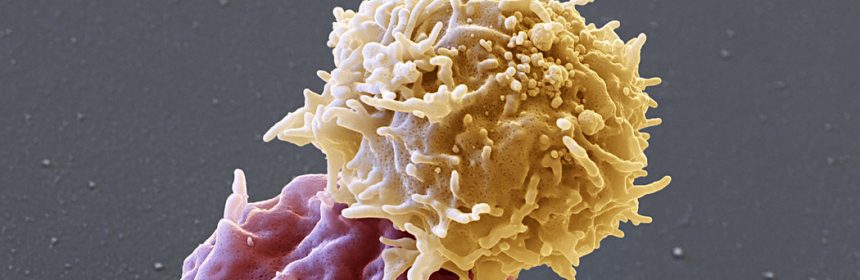
The treatment is a type of immunotherapy known as CAR-T, which has proved life-changing for some patients with blood cancers. CAR-T relies on engineered white blood cells — T cells — that seek out and destroy malignant cells in the body.
In the new study, published in the journal Nature, the technology was used to target scar tissue that stiffens the heart and prevents it from fully relaxing between beats in heart failure patients.
“It is potentially a breakthrough paper,” said Dr. Richard Lee, professor of stem cell and regenerative biology at Harvard who was not involved in the new study.
Medical experts like Dr. Lee agreed that the study is clever and innovative, and at least a proof of principle. But some asked if it would be feasible to use the therapy to treat heart patients, at least in the near future.
For cancer, CAR-T therapy costs about $450,000 per patient. When hospital stays are included, the price can soar to $1 million or more.
There are six million patients in this country with heart failure; even if the treatment at that price were offered to just a few of them, the overall costs would be astronomical.
Some patients getting CAR-T therapy experience severe, even fatal, side effects, including very high fevers, extremely low blood pressure and effects on the brain like confusion or seizures.
Deploying CAR-T against heart failure “is a really clever idea,” said Dr. Douglas Mann, a professor of medicine at Washington University in St. Louis. But given the cost of CAR-T and the side effects, he added, it is not practical today.
In heart failure, the walls of the ventricles, the two large pumping chambers, stiffen and may become enlarged, preventing the heart from pumping blood efficiently through the body. It may result from a number of conditions, including heart attack and high blood pressure.
While many patients respond to drug therapy, those with a type called heart failure with preserved ejection fraction have few treatment options. Half die within five years, a mortality rate comparable to that of some metastatic cancers.
Heart failure is a particular problem for people with muscular dystrophy, Dr. Lee noted. Heart failure, he said, “is a major life-limiting part of the disease.”
Heart muscle stiffens because of scarring, also called fibrosis, said Dr. Jonathan Epstein, lead author of the new study and professor of cardiovascular research at the University of Pennsylvania Perelman School of Medicine.
Fibrosis occurs in a range of other diseases: arthritis, chronic kidney disease and cirrhosis of the liver, for example. It results from the body’s response to inflammation. Although fibrosis is responsible for many of the worst symptoms of these diseases, it’s not clear what effect treating fibrosis might have.
The idea for the study originated with a student of Dr. Epstein, Haig Aghajanian. He wondered: Why can’t we make a CAR-T therapy to kill scar tissue in the heart?
He knew the way CAR-T works in cancer. T cells of the immune system are constantly scouring the body, looking for rogue cells to attach themselves to and kill. T cells sometimes do not recognize cancer cells, but researchers have found a way to fix that.
They attach a protein to T cells designed to lock on to the cancer. When these engineered T cells drift near a cancer cell, they latch on to it and kill it.
As long as most healthy cells do not have the docking site for that T cell protein, the treatment can work.
“It’s exciting,” said Dr. Elizabeth McNally, a cardiologist and human geneticist at Northwestern University Feinberg School of Medicine. But, she cautioned, there are several potential concerns for any therapy that attacks fibroblasts.
These are cells that help form all tissues, and they play a large role in wound healing. An ideal treatment shouldn’t eliminate fibrosis everywhere, only scars that hinder normal functioning.
So far, Dr. Epstein and his colleagues have not seen problems with wound healing or normal functioning in their animal subjects, but the work is experimental and preliminary.
Dr. Aghajanian and Dr. Epstein began by placing a docking site on scar tissue cells in the hearts of mice with heart failure. Then they made CAR-T cells that lock on to those sites.
Two weeks after the mice were treated, Dr. Aghajanian brought some slides to Dr. Epstein. The two sat side by side peering at them in the microscope. The heart tissue from the mice that were not treated was filled with scars. The heart tissue from the treated mice was clear.
“It was one of those ‘aha’ moments,” Dr. Epstein said. “We looked at each other and did a high-five over the microscope.”
The next step was to look for a naturally occurring protein that is present on human fibrosis cells but not on other cells. The group found one, fibroblast activation protein, or FAP, by looking through a large genetic database.
The scientists learned that mice and other animals also have FAP on scar tissue cells, so they engineered CAR-T cells to seek out the protein. The treatment worked to clear out scar tissue in the mouse hearts, and it did not seem to damage other tissue.
Now the investigators are beginning to repeat the experiment in dogs.
“I am hopeful we can move quickly to humans,” Dr. Epstein said, noting that a group in Germany has found a way to scan the hearts of heart attack patients and detect FAP.
That would allow doctors to know, quickly, if the patients are candidates for CAR-T.
As for the cost, he thinks it will come down. “First-generation cures are often expensive,” Dr. Epstein said. But “success and demand drive innovation.”
Jeffery D. Molkentin, executive co-director of the heart institute at Cincinnati Children’s Hospital Medical Center, is also optimistic that the obstacles can be overcome.
“It could be transformative,” he said.
“This whole idea of engineering T cells to attack cancer is just the tip of the iceberg,” he added. “What if we could engineer T cells to attack any cells in the body that cause trouble?”
Gina Kolata writes about science and medicine. She has twice been a Pulitzer Prize finalist and is the author of six books, including “Mercies in Disguise: A Story of Hope, a Family’s Genetic Destiny, and The Science That Saved Them.” @ginakolata • Facebook
Source: Read Full Article






