High levels of lipids in blood found to protect against allergies
People with relatively high levels of lipids in their blood are less likely to develop allergic conditions such as eczema and asthma. These lipids cause genes that play a key role in allergic reactions to be less active. Researchers from the Leiden University Medical Center (LUMC) have published an article about this in Nature Communications.
“We already knew that lipids in our blood, such as triglycerides and cholesterol, can influence the behavior of immune cells,” says Professor of Biomedical Data Sciences Bas Heijmans. “We have now shown that these lipids dampen the activity of genes that play a key role in allergies.” As a result, allergic reactions are less likely to occur.
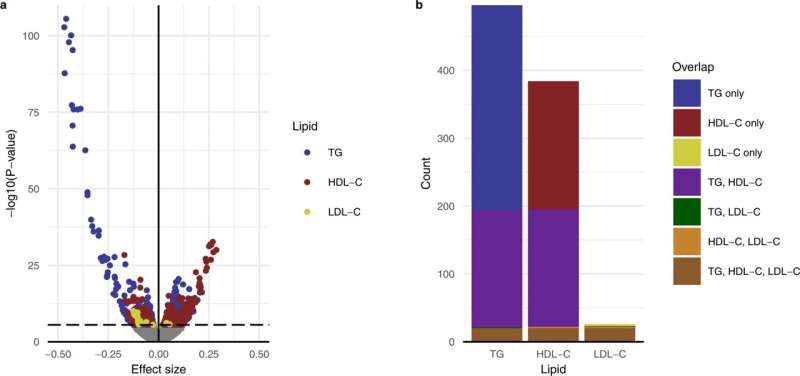
The researchers began by mapping which genes are active in the immune cells of over 3,200 people. “This turned out to be more than 17,000 genes,” says Koen Dekkers, the first author of the study. “Then, step by step, we figured out exactly which genes are affected by lipids in the blood, leading us to a group of genes that trigger allergic reactions.”
Using a cutting-edge analysis method that involved combining the blood levels of lipids, the activity of genes and known genetic differences between people, the researchers were able to show that this correlation is causal.
An allergic reaction is an exaggerated response by the immune system to a harmless substance. Take, for instance, how pollen can cause hay fever. The researchers found that lipids mainly affect genes active in basophils. These are immune cells that, among other things, produce histamine and are crucial in triggering an allergic reaction.
Saturated vs. unsaturated
Triglycerides in particular have an effect on these basophils, the researchers discovered. Blood triglyceride levels are determined partly by our DNA, but mainly by our diet. “And that is very interesting, of course,” says Heijmans. “This could mean that patients with severe allergic reactions might benefit from extra triglycerides, or more precisely, the fatty acids that make up triglycerides.”
But we are not there yet, Heijmans stresses. “We first need to test whether and, if so, which fatty acids actually have these beneficial effects. Is it mainly the healthy, unsaturated fatty acids? That would be good news. Or perhaps the unhealthy, saturated fatty acids?” It is also not clear yet how lipids change the behavior of immune cells in this way.
Unexpected outcome
Allergies were not exactly Heijmans and Dekkers’ area of expertise. “We did not expect at all that this study would point us in that direction,” says Dekkers. They had set their eyes on cardiovascular diseases, in collaboration with Professor of Cardiology Wouter Jukema. “These diseases are driven by the interaction between fats and the immune system,” says Heijmans.
“We expected to discover how lipids affect genes involved in cardiovascular disease. But the effect on allergic reactions was much stronger.” Their research had an unexpected outcome, but that hasn’t dampened their enthusiasm. “Such a surprising discovery is like icing on the cake for a scientist,” says Heijmans.
Will allergies now become a new focus within their research? Dekkers, who now works at Uppsala University in Sweden, does not rule it out for the longer term. “I definitely see follow-up research in it, and it could just be that I pick this up again later,” Heijmans says, “Wouter Jukema and I are as interested as ever in the effect of fats on immune cells, but are now focusing again on their role in cardiovascular disease.”
More information:
Koen F. Dekkers et al, Lipid-induced transcriptomic changes in blood link to lipid metabolism and allergic response, Nature Communications (2023). DOI: 10.1038/s41467-022-35663-x
Journal information:
Nature Communications
Source: Read Full Article