Forceps May Help Moms With Obesity Avoid Cesareans
Among patients who undergo forceps-assisted vaginal delivery, obesity does not appear to be associated with increased risk for complications such as injuries to the anal sphincter or the need for their babies to be admitted to the neonatal intensive care unit, researchers have found.
But obesity does appear to increase the chances that when physicians attempt operative vaginal delivery with either forceps or a vacuum, patients will wind up undergoing cesarean delivery, another study found.
Taken together, the new data may help inform physicians’ decisions about when to consider operative vaginal delivery as an alternative to emergency cesarean births.
Failed operative vaginal delivery ― that is, a cesarean delivery after an attempted operative vaginal delivery ― occurred for 10.1% of patients with obesity and 4.2% of those without obesity in a prospective study.
Researchers presented the findings last month at the Society for Maternal-Fetal Medicine (SMFM) 2023 Annual Pregnancy Meeting.
“We want to really try to reduce the rate of C-sections and primary cesarean deliveries. One of the ways to do that is to attempt operative vaginal delivery,” said Marissa Platner, MD, assistant professor of maternal-fetal medicine at Emory University School of Medicine in Atlanta, who was not involved in the new research.
Data on how obesity influences risks with operative vaginal delivery have been limited and mixed, the researchers said.
To examine how often attempted operative vaginal delivery fails in patients with obesity, Jennifer Grasch, MD, a maternal-fetal medicine fellow at the Ohio State University Wexner Medical Center in Columbus, and her colleagues conducted a secondary analysis of data from the Nulliparous Pregnancy Outcomes Study: Monitoring Mothers-to-Be, which included more than 10,000 participants.
“We know that cesarean sections among people with obesity are associated with increased complications, such as higher rates of infection and wound complications, than for people with lower BMI [body mass index],” Grasch said. “Operative vaginal delivery can be an alternative to cesarean delivery in some situations, so we were interested in whether attempted operative vaginal delivery was also associated with higher rates of complications in individuals with obesity than those without obesity.”
The researchers focused on 791 patients with an attempted operative vaginal delivery. About 40% had a BMI of 30 or greater. Clinicians used a vacuum in approximately 60% of the attempts.
After an attempted vacuum-assisted delivery, neonatal morbidity was more common for infants whose mothers had obesity than for those whose mothers did not (32.7% vs 22.3%; adjusted odds ratio, 1.61 [1.07 – 2.43]). Neonatal morbidity did not differ by obesity status following forceps-attempted delivery. Other adverse outcomes, including measures of maternal morbidity, did not significantly differ by obesity status, according to the researchers.
Choice May Come Down to Experience
Several factors influence whether a clinician chooses forceps- or vacuum-assisted delivery or cesarean delivery, “but one of the most important is experience,” Grasch said. “Complication rates with both forms of operative vaginal delivery are low, yet there has been a trend toward lower rates of both in the last few decades.”
Elizabeth Cochrane, MD, a maternal-fetal medicine fellow at Mount Sinai Hospital in New York City, and her colleagues investigated the relationship between obesity and adverse outcomes among patients with forceps-assisted vaginal deliveries.
The researchers analyzed data from 897 patients who underwent a forceps-assisted vaginal delivery between 2017 and 2021; 29% had a BMI of 30 or greater.
Injuries to the anal sphincter ― which can lead to fecal incontinence ― occurred in 18.7% of patients without obesity and in 17.7% of those with obesity. Admission to the neonatal intensive care unit occurred in 11.5% of patients without obesity and in 12.3% of patients with obesity. The differences were not statistically significant.
The bottom line: For forceps-assisted vaginal delivery, “obesity does not appear to be associated with increased rates” of adverse outcomes for mothers or newborns, the researchers concluded.
Reassuring Data
The study by Cochrane’s group “provides helpful information for providers to be reassured when they are performing forceps deliveries” for patients with obesity, Platner said.
Rates of obesity have risen in the United States, and physicians often wonder whether a patient with obesity could be a candidate for forceps-assisted delivery, Cochrane said. In 2019, 29% of women had obesity before becoming pregnant.
“It all really comes down to how comfortable the provider is in that skill set and also the overall clinical scenario,” she said. “Sometimes an operative delivery with forceps or a vacuum can be the fastest way to deliver a baby when there is acute concern for maternal decompensation or fetal decompensation.”
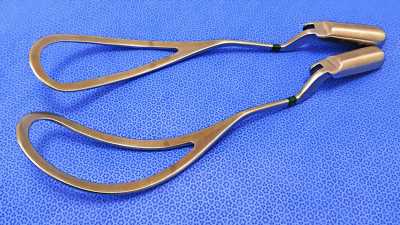
The alternative is an emergency cesarean delivery. Given that those operations can be riskier and more difficult for patients with higher BMIs, a forceps-assisted delivery may be “an interesting alternative to emergency caesarean sections, as long as it is in an appropriate clinical setting with providers who feel very confident and comfortable using those devices,” Cochrane said.
Society for Maternal-Fetal Medicine (SMFM) 2023 Annual Pregnancy Meeting.
For more news, follow Medscape on Facebook, Twitter, Instagram, and YouTube.
Source: Read Full Article