Each SARS-CoV-2 reinfection causes more severe disease
In a recent study under review at the Nature Portfolio journal and currently posted to the Research Square* preprint server, researchers at Washington University School of Medicine and VA Saint Louis Health Care System showed that acute severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) reinfection adds to the risks of all-cause mortality and hospitalization accrued during the first SARS-CoV-2 infection.
Background
Globally, people are acquiring repeat SARS-CoV-2 infections or reinfections. However, studies have not extensively investigated whether reinfection contributes to an increased risk of post-acute sequelae in the pulmonary and extrapulmonary organ systems and even death. Addressing these questions could reduce the overall burden of SARS-CoV-2 infections and inform reinfection mitigation and prevention strategies.
About the study
In the current study, researchers accessed the United States Department of Veterans Affairs electronic healthcare records (EHRs) to investigate how SARS-CoV-2 reinfection adds to the risk acquired after the first infection. They characterized the risks and 6-month burden of a panel of pre-specified outcomes in a cohort of people with first infection (n = 257,427), reinfection (2 or more infections, n = 38,926), and a non-infected control group (n = 5,396,855) to estimate risks and 6-month burdens of all-cause mortality, hospitalization, and a set of pre-specified incident outcomes.
The researchers presented two measures of SARS-CoV-2 reinfection-related risks. First, they assessed the adjusted hazard ratios (HRs) of pre-specified outcomes in re-infected people with those with a first SARS-CoV-2 infection. Second, they assessed the adjusted excess burden of each adverse clinical outcome of coronavirus disease 2019 (COVID-19) per 1,000 persons at six months of reinfection.
Lastly, the team performed positive and negative outcome control analyses. The positive outcome control analysis tested the association of a SARS-CoV-2 infection with the risk of fatigue, a well-characterized, key post-acute sequela of COVID-19. In the negative outcome control analyses, the researchers tested the association of a SARS-CoV-2 infection with negative outcome controls, such as atopic dermatitis and neoplasms.
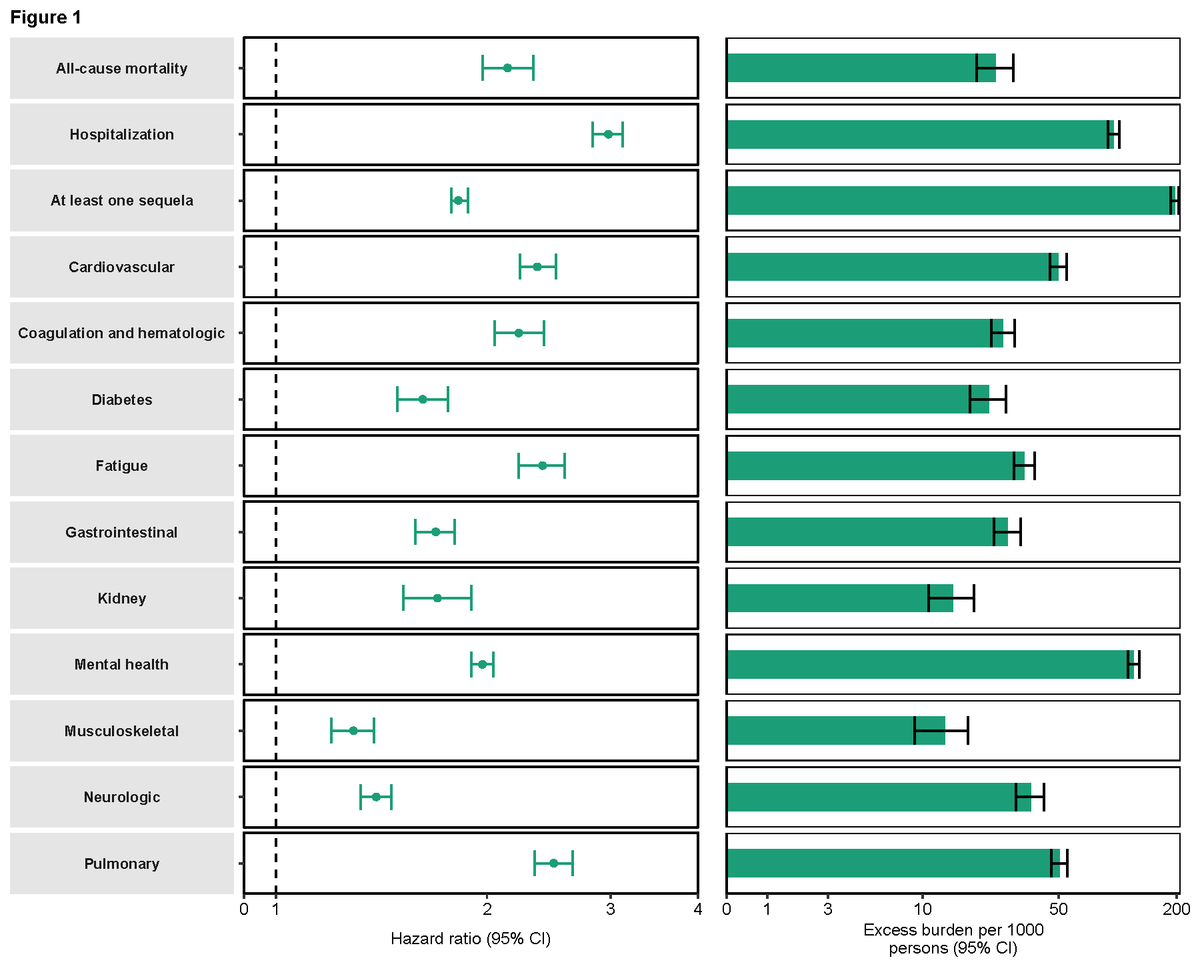
Risk and burden of sequelae in people with SARS-CoV-2 reinfection vs one infection. Risk and 6-month excess burden of all-cause mortality, hospitalization, at least one sequela, and sequelae by organ system are plotted. Incident outcomes were assessed from reinfection to end of follow-up. Results are in comparison of SARS-CoV-2 reinfection (n=38,926) to first SARS-CoV-2 infection (n=257,427). Adjusted hazard ratios (dots) and 95% confidence intervals (error bars) are presented, as are estimated excess burden (bars) and 95% confidence intervals (error bars). Burdens are presented per 1000 persons at 6 months of follow-up from time of reinfection.
Study findings
The study population had 257,427 participants who contracted COVID-19 only once and 38,926 participants with two or more SARS-CoV-2 reinfections. In the test group with reinfection cases, 12.29%, 0.76%, and 0.08% of people had two, three, and four or more infections, respectively. The median time distribution between the first-second and second-third infection was 79 and 65 days, respectively. Post-weighting, the standardized mean differences in the participant characteristics, including medications, diagnoses, and laboratory test results, remained balanced in each analysis.
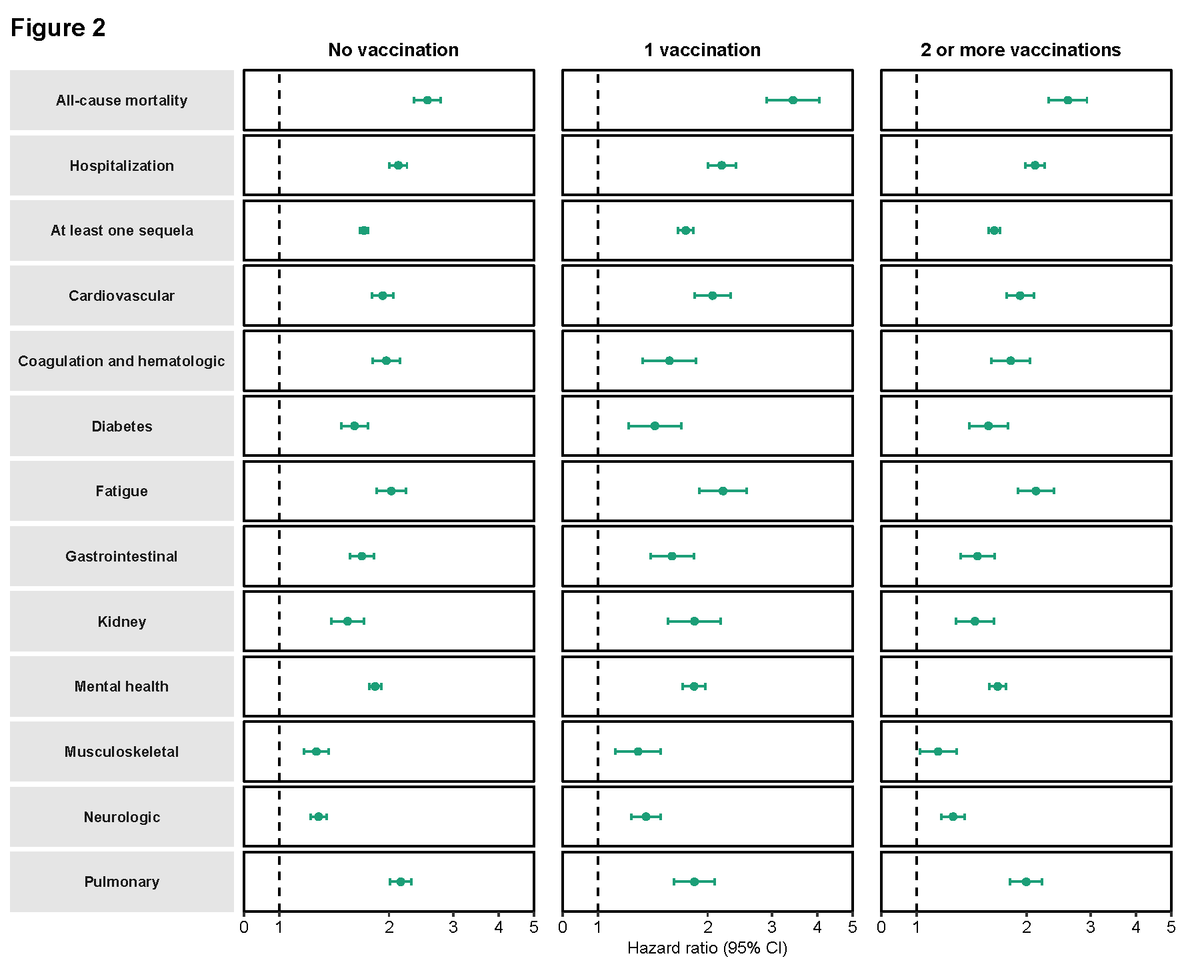
Risk and burden of sequelae in people with SARS-CoV-2 reinfection vs one infection by vaccination status prior to second infection. Risk of all-cause mortality, hospitalization, at least one sequela, and sequelae by organ system are plotted. Incident outcomes were assessed from reinfection to end of follow-up. Results are in comparison of SARS-CoV-2 reinfection (n=38,926) to first SARS-CoV-2 infection (n=257,427). At time of comparison, there were 69.49%, 9.09%, and 21.42% with no, one, and two or more vaccinations, respectively, among those with reinfection. At time of comparison, there were 59.86%, 9.18%, and 30.96% with no, one, and two or more vaccinations, respectively, among the first reinfection group. Adjusted hazard ratios (dots) and 95% confidence intervals (error bars) are presented.
Those with reinfections had a higher risk of all-cause mortality, with HR of 2.14 and an excess burden of all-cause mortality of 23.8 per 1000 persons at six months. These individuals also had a higher hospitalization risk, with an HR of 2.98. In addition, people with reinfection exhibited an increased risk of sequelae in the pulmonary and several extrapulmonary organ systems. Accordingly, reinfection increased the risk of adverse health outcomes in people with cardiovascular disorders, kidney problems, gastrointestinal issues, and musculoskeletal and neurological disorders. Overall, reinfection adversely impacted several extrapulmonary organ systems and the pulmonary system.
The positive outcome control analysis was based on prior biological and epidemiological evidence. Its results showed that compared to a non-infected control group, those with repeat SARS-CoV-2 infection exhibited an increased risk of fatigue (HR=2.02). Conversely, the risk of atopic dermatitis and neoplasms showed no such association. Furthermore, the time from initial infection to reinfection did not change the association between reinfection and the accrued risks of all-cause mortality, at least one post-acute sequela, and hospitalization, as indicated by the interactions on the multiplicative scale.
Conclusions
A SARS-CoV-2 reinfection, regardless of a person's vaccination status, increased the risk of all-cause mortality, hospitalization, at least one sequelae, and sequelae in different organ systems compared to the first infection. Although the risks were most pronounced in the acute infection phase, they persisted in the post-acute phase and up to six months for most sequelae. Moreover, the risk and burden of the pre-specified health outcomes increased in a graded fashion, with the lowest risk for people with one SARS-CoV-2 infection and the highest in people with three or more infections.
Over half a billion people have been infected with SARS-CoV-2 worldwide at least once. The study findings highlighted that continued vigilance is crucial for these people to reduce the overall risk to one's health. In addition, studies have gathered data that confirms that the reinfection risk is higher with the SARS-CoV-2 Omicron variant. The current study adds to the existing body of evidence, further validating that reinfection adds risk in both acute and post-acute phases among fully vaccinated people. This implies that combined natural and vaccine-induced immunity does not mitigate the risk following SARS-CoV-2 reinfection. In other words, regardless of COVID-19 history and vaccination status, people will need and benefit from reinfection prevention strategies.
*Important notice
Research Square publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
- Outcomes of SARS-CoV-2 Reinfection, Ziyad Al-Aly, Benjamin Bowe, Yan Xie, Research Square 2022, DOI: https://doi.org/10.21203/rs.3.rs-1749502/v1 https://www.researchsquare.com/article/rs-1749502/v1
Posted in: Medical Research News | Medical Condition News | Disease/Infection News
Tags: Atopic Dermatitis, Coronavirus, Coronavirus Disease COVID-19, covid-19, Dermatitis, Fatigue, Health Care, Healthcare, immunity, Kidney, Laboratory, Medicine, Mortality, Musculoskeletal, Omicron, Research, Respiratory, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Syndrome, Vaccine, Veterans Affairs

Written by
Neha Mathur
Neha is a digital marketing professional based in Gurugram, India. She has a Master’s degree from the University of Rajasthan with a specialization in Biotechnology in 2008. She has experience in pre-clinical research as part of her research project in The Department of Toxicology at the prestigious Central Drug Research Institute (CDRI), Lucknow, India. She also holds a certification in C++ programming.
Source: Read Full Article