Benefits of CRISPR-edited gene therapy for patients with blood disorders

In a late-breaking abstract presented at the European Hematology Association (EHA) Congress, a group of researchers that includes Children’s Hospital of Philadelphia (CHOP) presented new data on an investigational therapy for transfusion-dependent beta thalassemia (TDT) and severe sickle cell disease (SCD). The one-time treatment, developed by Vertex Pharmaceuticals and CRISPR Therapeutics, showed continued benefits at up to three years after administration, with a safety profile as expected for autologous transplant and potentially much safer than allogeneic transplant (from a donor).
“These data provide further evidence that this treatment has the potential to be transformational for patients with sickle cell disease and beta thalassemia,” said senior abstract author and immunotherapy pioneer Stephan A. Grupp, MD, Ph.D., Section Chief of the Cellular Therapy and Transplant Section and Inaugural Director of the Susan S. and Stephen P. Kelly Center for Cancer Immunotherapy at CHOP. “Although we must continue to investigate the durability of these results, I am excited about the current data.”
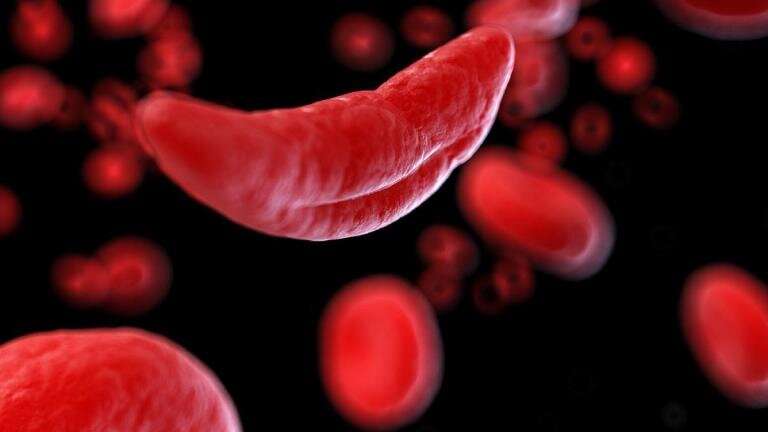
The abstract provides new data from two clinical trials on exa-cel (exagamglogene autotemcel), formerly known as CTX001, a one-time treatment that utilizes CRISPR gene editing to boost the production of fetal hemoglobin to correct the defective gene for hemoglobin associated with both diseases.
The researchers presented results from 75 patients: 44 with TDT and 31 with SCD. Of the 44 patients with TDT, 42 were transfusion-free at follow-up, which ranged from 1.2 to 37.2 months after exa-cel infusion. All 31 patients with SCD were free of vaso-occlusive crises at follow-up, which ranged from 2 to 32.3 months.
Source: Read Full Article