Adoption of Mediterranean diet shows promise in easing symptoms for myeloproliferative neoplasm patients

Myeloproliferative neoplasm (MPN) represents a group of inflammatory diseases, including polycythemia vera (PV), essential thrombocythemia (ET), and primary myelofibrosis (PMF). MPNs are linked to hematologic malignancies and are characterized by clonal outgrowth of hematopoietic cells with an acquired mutation in JAK2.
Multiple studies have shown that the Mediterranean diet positively impacts diseases associated with chronic subclinical inflammation. In addition to the Mediterranean diet, the gut microbiome also plays a crucial role in improving hematologic disorders.
A new study published to the medRxiv* preprint server assesses the feasibility of an education-focused Mediterranean diet intervention among MPN patients.


Background
Clinical manifestations of MPN include abnormal blood counts, thrombosis, and transformation to acute leukemia. One of the key characteristic features of MPN is increased plasma cytokines.
Chronic inflammation leads to abnormal blood count. Although JAK inhibitors alleviate MPN symptoms, these drugs are associated with certain risks, such as immunosuppression, skin cancer, and weight gain.
The recent National Comprehensive Cancer Network (NCCN) guidelines for MPN proposed several interventions to reduce symptom burden, irrespective of the prognosis scoring category.
Since many MPN patients do not meet the criteria for a cytoreductive agent, their symptoms are maintained without specific interventions. As a result, the quality of life of these patients is adversely affected due to the inability to limit disease progression.
Lifestyle modification, mainly through diet, can reduce inflammation. For example, a healthy diet high in anti-inflammatory agents can improve symptom burden among MPN patients. Adherence to this type of diet can decrease inflammation and significantly delay or prevent disease progression.
The Mediterranean diet is a primarily plant-based diet, which is associated with the consumption of nuts, extra virgin olive oil (EVOO), vegetables, fish, fruits, legumes, and whole grain products. Controlling inflammation through nutrition is a low-risk therapeutic approach to mitigate the burden of symptoms for MPN patients.
About the study
The primary aim of the current study was to determine the willingness of MPN patients to engage in dietary education to manage symptom burden. Participants were randomly assigned to either a standard U.S. Dietary Guidelines for Americans (USDA) group or Mediterranean diet group. Both groups received separate but equal education through written dietary resources and registered dietician counseling.
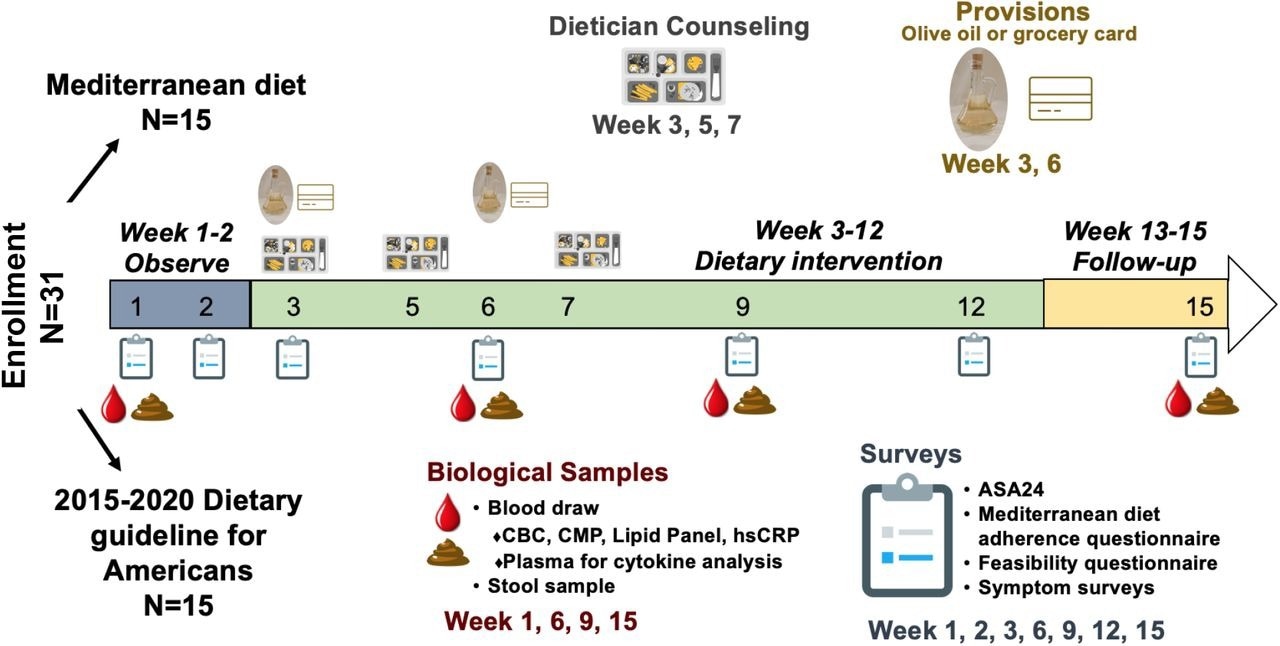
Patients were followed for adherence, feasibility, and symptom burden assessments. To explore changes in the gut microbiome and inflammatory biomarkers, biological samples were collected at four distinct time points throughout the 15-week study period.
NUTRIENT study design.
Study findings
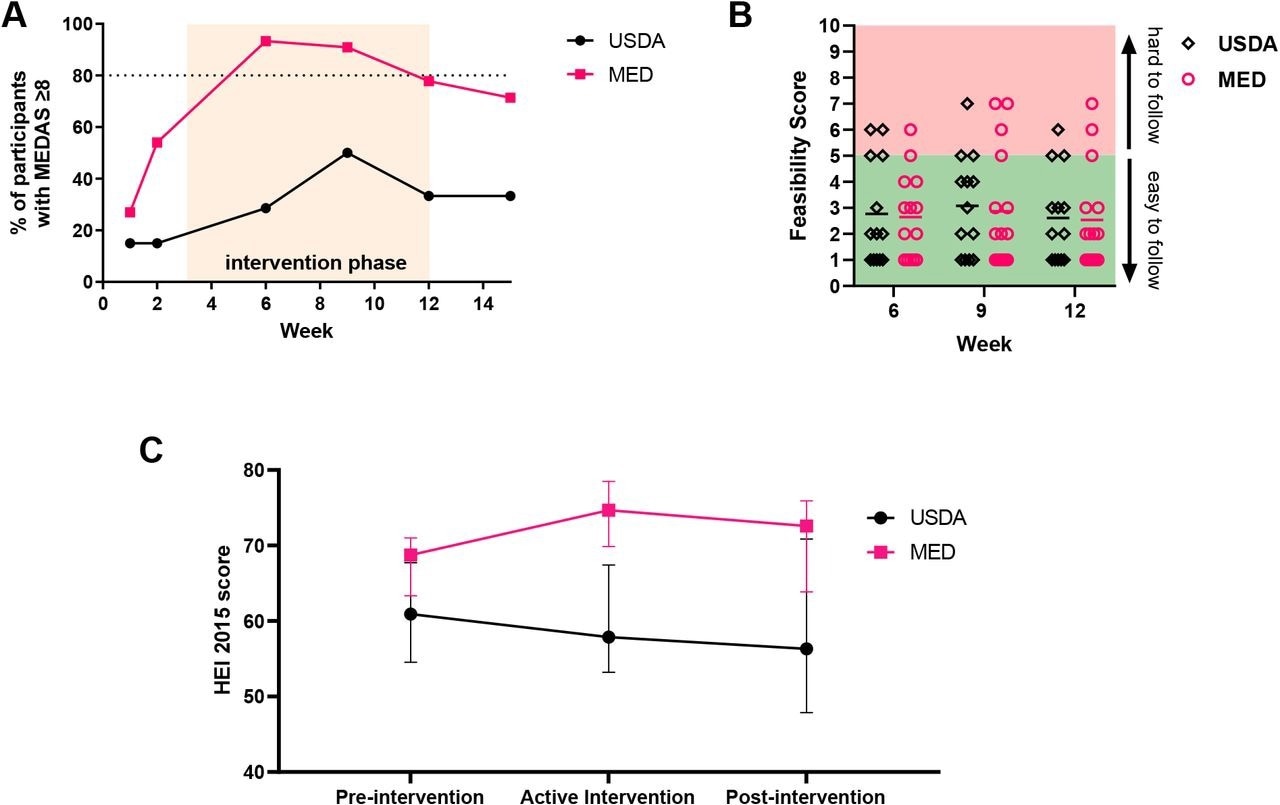
MPN patients found the Mediterranean diet program equally easy to follow as a program based on the U.S. Guidelines for Americans. Over 80% of participants in the Mediterranean diet group could maintain good adherence throughout the intervention period as compared to less than 50% in the USDA group. This serves as evidence that, with proper dietician counseling and written curriculum, MPN patients can feasibly adopt a Mediterranean diet.
MPN patients can adopt a Mediterranean eating pattern with dietician counseling and education. (A) Percentage of participant with MEDAS scores ≥8 at each time point with orange shaded area depicting the active intervention period (B) Participant responses to feasibility question during active intervention period (C) HEI-2015 was calculated from each 24 hour diet recall, and scores for each participant were averaged for the pre-intervention (weeks 1-2), active intervention (weeks 3-12), and post-intervention (weeks 13-15) period. Data shown represents median with interquartile range.
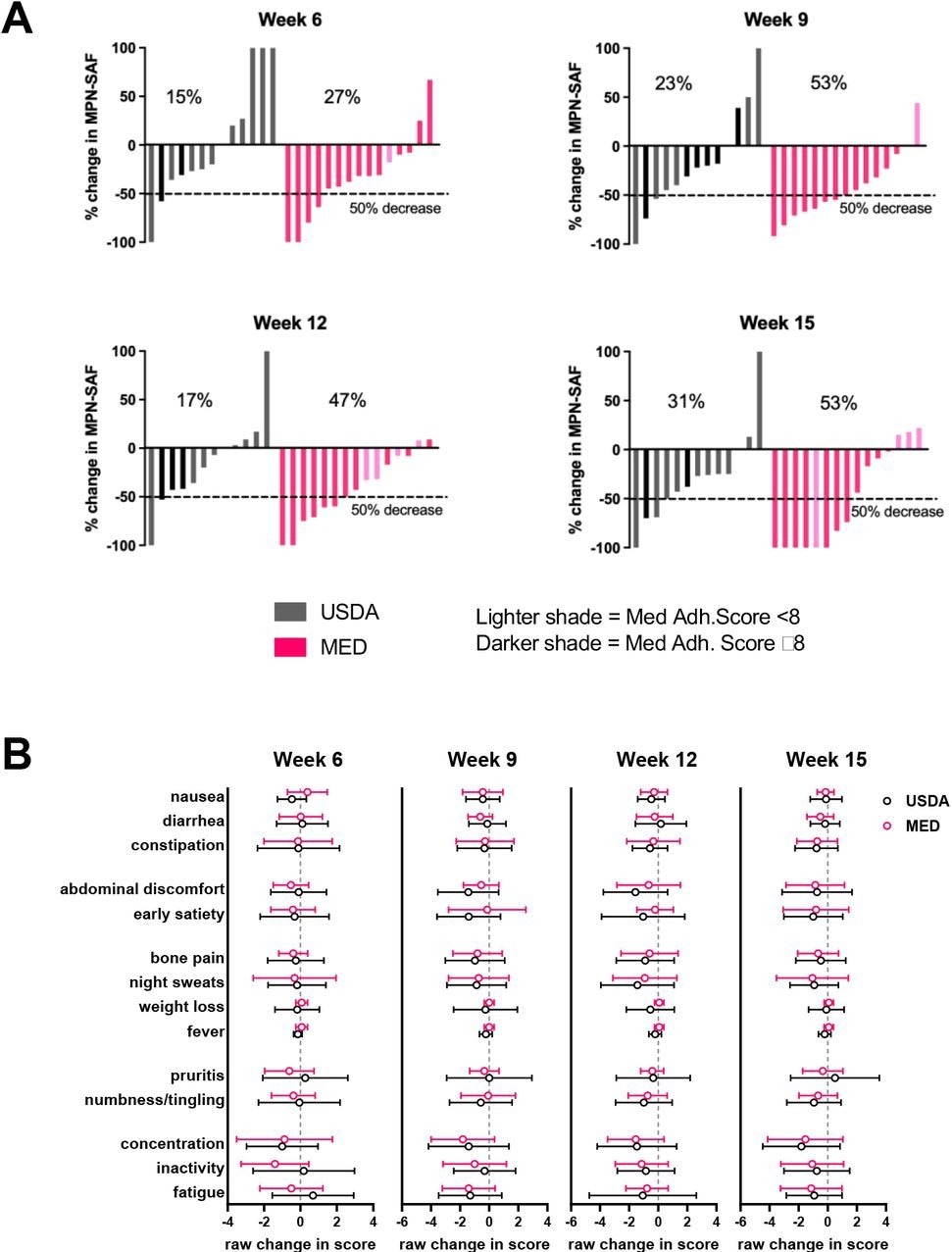
In MPN, an important goal is to target symptoms, as symptoms can significantly affect the patient’s’ quality of life. In the USDA group, 31% of the cohort exhibited more than a 50% reduction in the MPN-Total Symptom Score (TSS) at 15 weeks, whereas 53% of the Mediterranean diet group exhibited more than a 50% reduction in the MPN-TSS.
As compared to the USDA diet, the Mediterranean diet had a better effect on alleviating MPN symptoms. The length of the diet intervention and intensity are important factors in alleviating MPN symptoms.
Changes in symptom burden during study. (A) waterfall plots of percentage change in MPN-SAF (MPN-TSS) at each week compared to baseline (baseline defined as average MPN-TSS of weeks 1 and 2) (B) Raw change in specific symptoms at each week compared to baseline (mean±SD).
Future outlook
Both diets investigated in the current study led to a reduction in MPN symptom burden. Thus, these findings demonstrate that a 10-week intervention is sufficient to detect a change in symptoms.
In the future, a longer intervention period is required to assess whether improvements in symptoms continue. A longer intervention period would also help detect people with delayed symptom improvement.
The current analysis highlights that MPN symptoms may stem from different root causes; therefore, some symptoms change quickly compared to others. Due to the small sample size, a decrease in the inflammatory cytokines could not be detected. Therefore, future studies with a larger cohort are needed to elucidate how diets impact inflammatory cytokine levels.

- Preliminary scientific report. Luque, M. F. L., Avelar-Barragan, J., Nguyen, H., et al. (2023) The NUTRIENT Trial (NUTRitional Intervention among myeloproliferative Neoplasms): Feasibility Phase. medRxiv. doi:10.1101/2023.05.09.23289740
Posted in: Men's Health News | Medical Research News | Medical Condition News | Women's Health News | Disease/Infection News
Tags: Anti-Inflammatory, Blood, Cancer, Chronic, Cytokine, Cytokines, Diet, Drugs, Education, Essential Thrombocythemia, Fish, Immunosuppression, Inflammation, Leukemia, Microbiome, Mutation, Myelofibrosis, Neoplasm, Nutrition, Olive Oil, Polycythemia Vera, Primary Myelofibrosis, Skin, Skin Cancer, Thrombosis, Vegetables

Written by
Dr. Priyom Bose
Priyom holds a Ph.D. in Plant Biology and Biotechnology from the University of Madras, India. She is an active researcher and an experienced science writer. Priyom has also co-authored several original research articles that have been published in reputed peer-reviewed journals. She is also an avid reader and an amateur photographer.
Source: Read Full Article