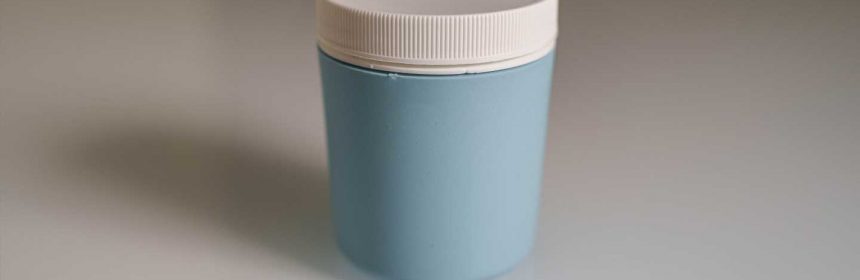
A specimen collection cup that creates a more favorable environment for sperm
Since 1978 when the world was introduced to the first baby conceived through in vitro fertilization (IVF), the procedure has become one of the primary assisted reproductive technologies, or ARTs used by the approximately one-in-seven U.S. couples that have trouble getting pregnant.
While as many as one in five pregnancy issues can be traced back to problems with the female egg, approximately 25% of these cases are linked to three main problems with the male: sperm count, sperm motility (movement) and the sperm’s morphology, or normal appearance.
To help address these male-related issues and raise the rate of successful pregnancies, Samuel Prien, Ph.D., and Lindsay Penrose, Ph.D., from the Department of Obstetrics and Gynecology at the Texas Tech University Health Sciences Center (TTUHSC) School of Medicine have worked for years to develop a specimen collection cup that creates a more favorable environment for the sperm.
Their efforts recently yielded a patent titled, “Method and Apparatus for Collection of Fluid Samples,” that makes important improvements to the first patented collection cup invented at TTUHSC by Prien and Dustie Johnson, Ph.D. That device, known as the DISC (Device for Improved Semen Collection), is sold by RSI Technologies under the brand name ProteX.
“Basically what it does is it tries to keep the sperm from thinking they’ve left the male body; it protects the sperm as it would be protected inside the male body,” Prien explained. “It keeps it at approximately the right temperature and it doesn’t let it get shocked by a lot of the other influences present in a normal specimen cup.”
Prien said a typical human semen sample contains about a teaspoon of material. When placed into a standard specimen cup, it spreads out across the bottom of the cup and very quickly cools as it makes contact with the plastic. The sample also is exposed to additional air, which oxidizes and damages the sperm. The original DISC creates an environment where the sample is pooled into the smallest exposed surface area possible. The cup confines the sample so that it dictates its own temperature, and its exposure to oxygen is significantly reduced.
“The new version of the DISC has added additional levels of protection to prevent biochemical damage to the cells,” Prien said. “These new properties lower the chances of sperm damage during processing, especially its DNA. Providing the best collection environment should lead to healthier sperm; healthier sperm should make the best embryos, and the best embryos should result in more babies for couples seeking reproductive treatment.”
In cases where an ART procedure is required, Prien said the DISC provides a better overall sperm sample, which increases the couple’s chances for a successful pregnancy. Using the original DISC results in a sperm sample that has more motility over a longer period of time than a sample collected in a standard cup. Because this increases the availability of a functional sperm pool, it can mean the difference between a doctor being able to perform a simple, low-cost procedure (e.g., intra-uterine insemination) at a cost of a few hundred dollars verses requiring a couple to go through a “high-tech” procedure such as IVF at a cost of tens of thousands of dollars.
However, Prien said, one of the things the original DISC did not do very well was to protect the DNA in the sperm cells. Free oxygen radicals in the environment, whether from the male’s own seminal fluid or from other environmental factors such as the plastic in the cup, has a negative effect on the sperm because it basically ruptures the sperm’s DNA molecules.
To reduce the chances of DNA damage, practitioners have for years tried to add anti-oxygen fluids to specimen cups in hopes the resulting sperm will be sufficient. Unfortunately, that doesn’t work very well. In fact, Prien said, that may be worse for the sperm than having no protection at all because sperm need a small amount of free oxygen radicals to cause chemical reactions. He compared it to the Goldilocks dilemma where too much is bad and too little is bad, so it needs to be just right.
“You’re too high, then you’re too low, and the sperm don’t like that,” Prien said. “By doing what we’ve done with this latest patent, which is to incorporate the antioxidant directly into the plastic, the plastic serves as a sink. Extra free oxygen radicals are gobbled up by the plastic, so you keep them at just the right level and the DNA doesn’t get damaged, at least from the studies we’ve done. It’s not that we’re making the new DISC a certain percentage better than the original, it’s that we’re adding in a whole new layer of protection for the sperm cells.”
Providing patients with the healthiest sperm sample possible is the primary point of creating the original DISC and making improvements to the second edition of the collection system. Penrose said there is some data out now that shows that while the pregnancy rate is the same using the ProteX cup, approximately 25% more couples are experiencing successful births. In other words, the quantity of pregnancies hasn’t increased, but the quality of the pregnancies has significantly improved.
“What that is telling us is that an embryo will implant because that’s what embryos do, but not all embryos will become a baby,” Penrose stressed. “That’s our goal: to have patients take home babies, so I’m very excited to see this new patent come into use because DNA fragmentation is a big issue in our field. If you don’t have good DNA, you’re not going to make a good embryo. It’ll implant but you won’t get a baby.”
Now that they have a patent for the second-generation DISC, Penrose is looking forward to conducting clinical trials using their new technology. She hopes the new device will improve upon the 25% increase in take-home babies that the original DISC produced.
Source: Read Full Article

