nolvadex blog

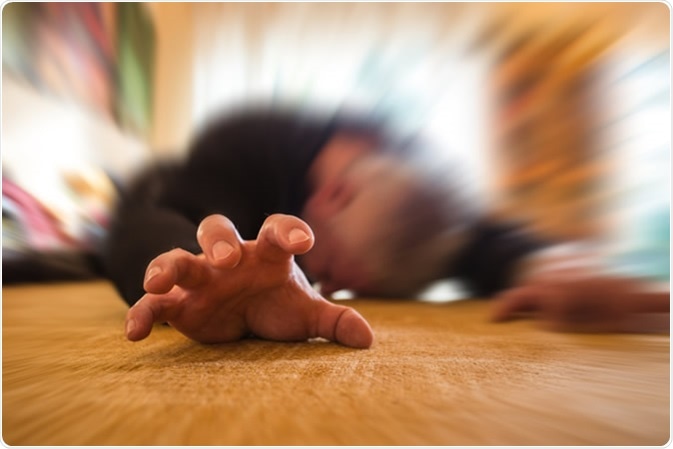
Epilepsy is a neurological condition characterised by recurrent episodes of seizures. Most cases of epilepsy do not have a clear known cause, apart from susceptible genetic factors.
The primary pathogenesis of genetic forms of epilepsy is an abnormal expression of certain receptors in the brain that lead to an enhanced excitation and reduced inhibition. Some cases occur following oxygenation deprivation during birth.
Other later-life forms of epilepsy may be attributed to damage to the brain e.g. stroke, brain tumours, traumatic brain injury, drug misuse or a brain infection.
To date, there are several key treatment strategies to help people have fewer seizures. Predominantly, anti-epileptic drugs are used to treat the frequency and severity of epilepsy. However, these have to be taken routinely, and are not a long-term solution. They also have many undesired side-effects. However, anti-epileptic drugs may not work for everyone, therefore other treatments are used, including surgery and dietary modifications (e.g. keto-diet). Therefore, the need to find effective long-term solutions is needed to treat epilepsy.
What are Stem Cells?
Stem cells are cells that have the ability to develop into different specialised cell types of the body. Most cells in the body are post-mitotic, meaning they are unable to divide and grow into new types of tissues. However, stem cells are able to divide after periods of no apparent activity and are able to transform into different body cell types, including muscle cells, nerve cells and blood cells.

Stem cells therefore have the potential to be used in the treatment of many disorders where the normal body cells are dysfunctional or abnormal. This includes conditions where the body’s own cells begin to degenerate e.g. stroke, heart attacks, spinal cord injury and macular degeneration.
Traditionally, stem cells were only able to be isolated from embryos (animal and human) and some adult somatic stem cells, such as those found in e.g. bone marrow. However, due to advances in science and technology, adult cells taken from tissues such as e.g. skin, are now able to be reprogrammed into stem-cell like cells called induced pluripotent stem cells (iPSCs). These iPSCs may be able to function in very similar ways to those previously only obtainable through embryo donation.
iPSCs can be genetically manipulated to form a variety of different body cells e.g. neurons and muscle cells. However, much more work is needed before iPSCs can be used to replace dysfunctional cells within the body, though many advances have been made, especially in animal studies, including successful replacement of damaged heart cells with lab grown heart cells from the animals.
Can Stem Cells be Used to Treat Epilepsy?
As most cases of epilepsy can be attributed to receptor expression differences within the brain (due to mutations), correcting these may in theory reduce the likelihood of electrical seizures developing in the brain.
In addition, during status epilepticus, the excitation overload sometimes kills neurons, especially within the hippocampus. This can actually worsen the condition over time and lead to the development of temporal lobe epilepsy (TLE). Whilst anti-epileptic medication may treat the seizures, the damage caused to the temporal lobe is often irreversible and permanent, and current therapies do not address this.
As previously discussed, the reduction in inhibition in the brain, primarily due to loss of GABA-ergic interneurons, coupled with increased excitation of neurons, is key in the development of epilepsy including TLE.
Scientists therefore have speculated that enhancing inhibition by GABA-neurons may alleviate status epilepticus due to renewed inhibitory balance.
A study by Upadhya and colleagues (published in 2019 in PNAS); aimed to investigate whether iPSCs grafted into the brain of rats could reduce seizures and reverse damage in the hippocampus. They found that medial ganglionic eminence (MGE) cells derived from human-derived iPSCs, grafted into the hippocampus successfully reduced the frequency of seizures and reduced GABA-ergic neuronal loss.
Furthermore, there was an improvement to cognition and mood. Although this study was performed in rats, the implications of this research has far reaching potential to be used clinically.
Another study, a Phase I clinical trial in 22 patients, using autologous mesenchymal stem cells in epilepsy patients was shown to reduce overall seizure frequency (published in Advances in Medical Sciences by Hlebokazov and colleagues in 2017). Stem cells were obtained from patients’ own bone marrow, and administered intravenously and through a single injection into the spinal cord. After 1 year, 3 out of 10 patients achieved complete remission (no seizures) and another 5 patients that previously did not respond to drugs began to respond favourably. No side effects were observed in any of the patients.
This study is promising and showed a good safety profile for the patients. It appears that stem cells were associated with alleviation of pathological hallmarks as well as the symptoms of epilepsy. Though this was only a Phase I trial with a very small cohort, additional controlled trials with placebos are needed in a larger cohort to make any definitive conclusions on the efficacy and safety.
In summary, stem cell based therapies, show promising results in the treatment of diseases including epilepsy. Animal and clinical studies have shown the remarkable efficacy of stem cells’ regenerative properties. However, larger clinical trials are needed before stem cell therapy can become routine. It is also expensive with therapies starting at around $5,000-$8,000 per treatment, though they can be as expensive as $25,000. In the UK, the NHS does not offer stem cell therapy routinely, only for a very small number of people in designated centres for diseases such as MS.
In the United States, the only type of stem cell therapy that has been extensively studied and approved for human treatment involves use of hematopoietic stem cells for patients with certain types of cancer.
Sources:
- NHS.uk, 2019. Epilepsy. https://www.nhs.uk/conditions/epilepsy/
- NIH.gov, 2019. Stem Cell Information. https://stemcells.nih.gov/info/basics/1.htm
- Upadhya et al, 2019. Human induced pluripotent stem cell-derived MGE cell grafting after status epilepticus attenuates chronic epilepsy and comorbidities via synaptic integration. PNAS. 116(1):287-96. https://www.pnas.org/content/116/1/287.short?rss=1
- Hlebokazov et al, 2017. Treatment of refractory epilepsy patients with autologous mesenchymal stem cells reduces seizure frequency: An open label study. Adv Med Sci. 62(2):273-279. https://www.ncbi.nlm.nih.gov/pubmed/28500900
Further Reading
- All Epilepsy Content
- What is Epilepsy?
- Epilepsy Classification
- Epilepsy Epidemiology
- Epilepsy Pathophysiology
Last Updated: Jul 5, 2019

Written by
Osman Shabir
Osman is a Neuroscience PhD Research Student at the University of Sheffield studying the impact of cardiovascular disease and Alzheimer's disease on neurovascular coupling using pre-clinical models and neuroimaging techniques.
Source: Read Full Article