New vaccine offers fresh take on malaria fight
Early research on a new approach to protecting against malaria is offering promising, potentially long-lasting results against the persistent parasite that sickens hundreds of millions people each year.
The approach uses a cytomegalovirus-based platform that’s already being used in vaccines being developed to battle HIV and tuberculosis. This new vaccine reduced the malaria-causing parasite’s release from the liver and into the blood of infected rhesus macaques by 75 to 80 percent, reports a paper published in the journal PLOS ONE.
“The problem with most vaccines is that their effectiveness is often short-lived,” said the study’s lead author, Klaus Früh, Ph.D., of OHSU’s Vaccine & Gene Therapy Institute and a professor of molecular and cellular biosciences at the OHSU School of Medicine. “Our cytomegalovirus-based vaccine platform can create and keep immunity for life. With further research and development, it could offer a lifetime of protection against malaria.”
Malaria is a serious and sometimes fatal disease caused by Plasmodium parasites, which are spread to humans through mosquito bites. It can cause high fevers, shaking chills, flu-like illness and, in the worst cases, death. Worldwide, 216 million people were infected with malaria in 2016, leading to 445,000 deaths. The vast majority of infections occur in Africa.
The decades-long search for an effective malaria vaccine has been challenging. The World Health Organization is using one vaccine—known as RTS,S/AS01 or by its brand name, Mosquirix—as part of new, routine vaccination programs in three African countries. But RTS,S has been shown to only reduce malaria transmission in kids—in whom malaria is most often fatal—by 39 percent four years after it was administered. Its efficacy was further reduced to 4.4 percent seven years afterward. Vaccines against viruses and bacteria typically have protection rates of more than 90 percent.
Vaccine makeover
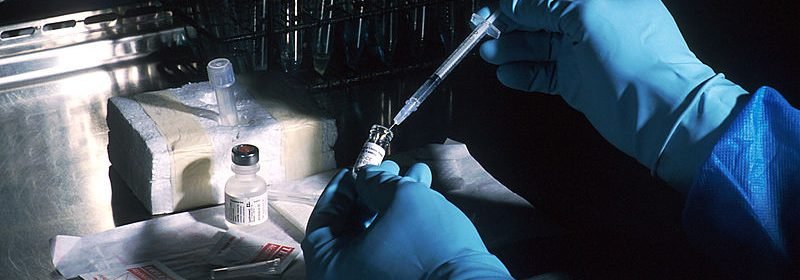
Most vaccines are designed to encourage the human body to respond to invading, disease-causing pathogens by creating antibodies that disable those pathogens. OHSU’s new vaccine takes a different approach by using a weakened form of a common herpes virus—cytomegalovirus, or CMV—that infects most people without causing disease.
Früh and his colleagues weave tiny bits of their target pathogen into CMV. Those who receive the resulting, re-engineered CMV vaccine produce memory T-cells that can search for and destroy pathogen-infected cells. Studies have shown this approach enables vaccinated nonhuman primates to develop and maintain a high state of immunity years later.
The CMV vaccine platform has been licensed by Vir Biotechnology, Inc., of San Francisco, which plans to lead a human clinical trial for a CMV-based HIV vaccine in 2019. The same basic platform is also being used in a new TB vaccine, and is now the basis for this malaria vaccine.
Nuts & bolts
Früh and his colleagues pursued a malaria vaccine because they noticed the memory T-cells their CMV-based vaccine produce exist in high concentrations in the liver, where the malaria parasite hides out shortly after infecting a human.
They developed two different versions of their CMV-based malaria vaccine while using four different proteins made by the Plasmodium parasite. The resulting vaccines delayed the parasite’s appearance in the blood of 16 infected and vaccinated rhesus macaques by eliminating between 75 and 80 percent of parasites from the liver. A year later, the vaccinated nonhuman primates still had immunity against malaria, while eight control animals that weren’t vaccinated did not.
Source: Read Full Article
