Venetoclax Combos Improve Progression-Free Survival in CLL
Use of the targeted therapy combination of venetoclax plus obinutuzumab for fit patients with chronic lymphocytic leukemia (CLL) significantly improved progression-free survival (PFS) at 3 years compared with standard chemoimmunotherapy, new phase 3 data show.
Adding the BTK inhibitor ibrutinib to the two-drug combination pushed the 3-year PFS even higher, but the risk of severe adverse events may outweigh the benefits of the triple combination for some higher-risk patients.
“Time-limited targeted therapy with venetoclax plus obinutuzumab, with or without ibrutinib, is superior to chemoimmunotherapy with respect to progression-free survival,” said first author Barbara Eichhorst, MD, of the University of Cologne, Cologne, Germany.
However, given higher rates of infection and other adverse events observed when adding ibrutinib, “I would say, based on this data, not to use the triple combination in clinical practice,” Eichhorst cautioned.
Eichhorst presented the late-breaking results on June 12 at the European Hematology Association (EHA) 2022 Annual Meeting in Vienna.
For patients considered unfit for chemoimmunotherapy, the fixed-duration therapy of venetoclax plus obinutuzumab has become standard treatment for CLL. For those deemed fit to withstand chemoimmunotherapy, this option remains the standard of care.
However, no studies have compared the targeted combination to chemoimmunotherapy for fit patients with CLL.
Eichhorst and her colleagues conducted the GAIA/CLL13 trial to determine how the two- or three-drug targeted combinations stack up against standard chemoimmunotherapy for fit patients.
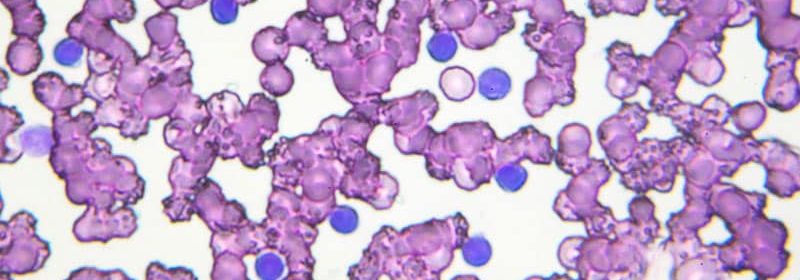
In the phase 3 study, 920 treatment-naive, fit patients with CLL in which there were no TP53 aberrations were randomly assigned to one of four treatment groups that each had 230 patients — standard chemoimmunotherapy or one of three time-limited venetoclax arms. The regimen for the chemoimmunotherapy group included fludarabine, cyclophosphamide, and rituximab for those aged 65 and younger, and bendamustine and rituximab for those over 65. The patients who received venetoclax were divided into groups that received either venetoclax plus rituximab, venetoclax plus obinutuzumab, or triple therapy of venetoclax, obinutuzumab, and ibrutinib.
The median age was 61, and follow-up was just over 3 years (38.8 months). Nearly 40% of patients were in advanced Binet stages, and more than half (56%) were of unmutated immunoglobulin heavy-chain gene (IgHV) status, which is associated with worse outcomes in CLL.
Compared with chemotherapy, the two-drug combination demonstrated significantly better PFS (hazard ratio [HR], 0.32; P < .000001), as did the triple therapy (HR, 0.42; P < .001), though the venetoclax-rituximab combination did not (HR, 0.79; P = .183).
The 3-year PFS rates were highest in the triple-therapy group (90.5%), followed by the venetoclax and obinutuzumab group (87.7%). The chemoimmunotherapy (75.5%) and venetoclax plus rituximab groups (80.8%) had the lowest 3-year PFS rates.
Overall, 3-year PFS rates for patients with unmutated IGHV were slightly lower compared with those who had mutated IGHV.
The best PFS rate was among patients who received the three-drug combination, although one interesting caveat emerged among the under-65 subset of patients in the mutated IGHV group: the chemotherapy arm achieved a slightly better PFS rate (95%) compared with the triple-therapy arm (93.6%).
Notably, overall survival was similar among all groups; about 96% of patients were alive at 3 years.
Several adverse events were more pronounced in the triple-therapy group. The highest rate of grade 3 to 4 infections was among those who received ibrutinib (22.1% vs 20.4% for chemotherapy, 11.4% for venetoclax/rituximab, and 14.9% for venetoclax/obinutuzumab). The triple-therapy group also had the highest rate of hypertension (5.6% vs 1.4% for chemotherapy, 2.1% for venetoclax/rituximab, and 1.8% for venetoclax/obinutuzumab).
Rates of febrile neutropenia and secondary primary malignancies, however, were highest in the chemoimmunotherapy group. More than 11% of patients in the chemoimmunotherapy group had febrile neutropenia, compared with 7.8% of those who received triple therapy, 4.2% in the venetoclax/rituximab group, and 3.1% of those whor eceived venetoclax/obinutuzumab. Almost half of patients in the chemoimmunotherapy group had secondary primary malignancies, vs fewer than 30% in the other arms.
EHA President-Elect António Almeida, MD, noted that the research sheds important light on evolving treatment options for CLL.
“The first is that the triple combination appears better than the double combinations, and I think that’s an important message because of longer treatment-free remission and progression-free remissions,” Almeida, of the Hospital da Luz, in Lisbon, Portugal, told Medscape Medical News.
The second important message: Given the time-limited administration of the venetoclax combinations, the data show that “we can stop ibrutinib and that is safe,” he added. “That’s quite important.”
Third, the findings can help guide treatment choices. “We’ve already had an indication that obinutuzumab is better than rituximab in the CLL setting, but this again solidifies that notion,” Almeida added.
Eichhorst has relationships with Janssen, Gilead, F. Hoffmann-La Roche Ltd, AbbVie, BeiGene, AstraZeneca, MSD, Adaptive Biotechnologies, and Hexal. Almeida has disclosed no relevant financial relationships.
European Hematology Association (EHA) 2022 Annual Meeting: Abstract LB2365. Presented June 12, 2022.
For more news, follow Medscape on Facebook, Twitter, Instagram, and YouTube.
Source: Read Full Article