TMVR Benefit for Severe Mitral Regurgitation Durable at 2 Years
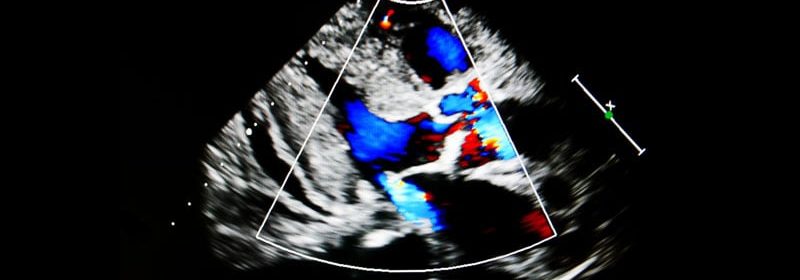
The positive effect of transapical transcatheter mitral valve replacement (TMVR) in patients with severe symptomatic mitral regurgitation (MR) is sustained at 2 years, according to follow-up data on the first 100 patients from the Expanded Clinical Study of the Tendyne Mitral Valve System (Abbott Vascular).
The results of the open-label, nonrandomized, prospective study were published online November 8 in JACC: Cardiovascular Interventions.
Noting that their study extends previously reported outcomes at 1 year for patients treated by the Tendyne TMVR device, David W.M. Muller, MBBS, MD, St. Vincent’s Hospital, Sydney, NSW, Australia, and colleagues report that TMVR was associated with a low mortality and reduced the need for hospitalization for heart failure between 1 year and 2 years postoperatively in a population at high risk for conventional mitral valve surgery.
In addition, the “near elimination of MR that was observed at 1-year follow-up was sustained to 2 years with no apparent structural valve deterioration, as were improvements in functional status and quality-of-life,” they write.
“Severe mitral regurgitation is a common problem that can often be treated by surgical valve repair or replacement, but for surgically ineligible patients, the prognosis is poor,” Muller told theheart.org | Medscape Cardiology.
“Over the past decade, less invasive approaches to treating mitral valve disease have been developed. These include transcatheter mitral valve replacement (TMVR). The Tendyne valve is one such device. The first cases were done more than 6 years ago,” he said.
The main message is that TMVR is feasible in a high-risk population of patients who are poor candidates for surgery and transcatheter valve repair, “with very good intermediate term results,” Muller said.
The results should promote confidence in the use of the device, he added.
The valve is commercially available in Europe, Muller noted. It is also being tested in a randomized trial against transcatheter edge-to-edge repair (TEER). “This will help define the role of TMVR in patients who are eligible for both TMVR and TEER,” he said. “The main challenge now is to identify the parameters that will help selection of the best treatment strategy for patients with severe MR who are poor candidates for surgery.”
The patients (69% men) ranged in age from 55 to 91 years, were symptomatic with 3+ or 4+ MR, and were considered high-risk surgical candidates, with comorbidities that included diabetes (38%), atrial fibrillation (35%), coronary artery disease (74.0%), previous coronary bypass graft surgery (47%), and previous stroke or transient ischemic attack (14%).
At baseline, 10 (10%) patients had biventricular pacemakers and 23 (23%) had implantable cardioverter-defibrillators. They were deemed to be high-risk surgical candidates, with a mean Society of Thoracic Surgeons Predicted Risk of Mortality of 7.8%.
All patients were symptomatic; 62% were New York Heart Association (NYHA) functional class III.
The procedure was performed through a transapical approach, and the valve prosthesis was delivered through a 36-F sheath.
Mixed MR was present in 89% of patients, and the mean left ventricular ejection fraction was 46.2% at baseline.
The valve prosthesis was successfully implanted in 97% of patients. There were no deaths during the procedure, but six patients died before hospital discharge.
At 2 years, nine patients had withdrawn from the study, 39 patients had died, and three patients missed their follow-up visit. The remaining 49 patients completed the 2-year follow-up.
At 2 years, all-cause mortality was 39.0%, with a cardiovascular mortality of 34.0%. All-cause mortality was highest 3 months after the procedure. Of the 39 deaths at 2 years, 17 (43.6%) occurred in the first 90 days. The remaining 22 (56.4%) occurred between 90 days and 2 years.
The predominant causes of death during the first 90 days were refractory heart failure in 11 patients and fatal arrhythmias in five patients.
In all, 37 patients required hospitalization for heart failure at 2 years, with 21 heart failure hospitalizations occurring during the first 90 days and 24 events between 90 days and 2 years.
Heart failure hospitalization fell from 1.30 events per year before the procedure to 0.51 per year in the 2 years post TMVR (P < .0001).
At 2 years, 93.2% of surviving patients had no MR. No patient had >1+ MR.
In addition, the improvement in symptoms seen at 1 year, with 88.5% achieving NYHA functional class I or II, was sustained at 2 years, with 81.6% of patients maintaining NYHA functional class I or II.
Among survivors, the left ventricular ejection fraction was 45.6 ± 9.4% at baseline and 39.8 ± 9.5% at 2 years (P = .0012). Estimated right ventricular systolic pressure decreased from 47.6 ± 8.6 mm Hg to 32.5 ± 10.4 mm Hg (P < .005)
Important Information for an Emerging Field
“This work provides important additional information to the emerging TMVR field, particularly considering the paucity of data on intermediate-term outcomes following TMVR,” Josep Rodés-Cabau, MD, PhD, Quebec Heart & Lung Institute, Laval University, Quebec City, Canada, and colleagues write in an accompanying editorial comment.
“However, the relatively high rate (>10%) of patients lost to follow-up along with the echocardiographic availability in <50% of cases at 2 years (despite that follow-up echocardiography was performed in approximately 90% of patients at risk) were important limitations of the study that may indeed have biased the final results, especially considering the relatively small sample size,” they write.
“This is one of the first studies in the TMVR field to provide data beyond 1 year follow-up,” Rodés-Cabau told theheart.org | Medscape Cardiology.
“The high mortality rate, 39%, with a significant number of patients dying within the first months following the procedure, reflects the high-risk profile of the patients undergoing TMVR nowadays and highlights the importance of careful patient selection. Also, a potential negative impact of the transapical approach, including myocardial injury, thoracotomy complications, potential hemostatic issues, cannot be excluded,” he said.
The data on valve performance at 2 years are “reassuring,” Rodés-Cabau said, but with one fourth of patients exhibiting major, life-threatening bleeding events and thrombotic complications, bleeding complications are concerning.
“Further studies are urgently needed to determine the optimal type and duration of antithrombotic therapy in this field,” he said.
Two-Year Outcomes Encouraging, However…
“The 2-year outcome data from the randomized study of the Tendyne mitral valve prosthesis are encouraging,” Catherine M. Otto, MD, professor of medicine, University of Washington, Seattle, commented to theheart.org | Medscape Cardiology.
“However, these data are applicable to only a small subset of patients ― those with high surgical risk, very symptomatic severe mitral regurgitation, and a left ventricle that is not excessively dilated, with diastolic diameters less than 70 mm, or excessively dysfunctional, with an ejection fraction less than 30%,” Otto said.
“In addition, this procedure is not really noninvasive ― general anesthesia and an, albeit small, thoracotomy are needed,” she noted. “Finally, this is an observational study with no comparison arm; although there was a lower annual rate of hospitalization after the intervention, mortality was very high, reaching 39% at 2 years, suggesting a marginal overall benefit which needs to be balanced against risk and cost.”
The study was supported by Abbott. Muller reports financial relationships with Medtronic, Abbott, and Edwards Life Sciences. Rodes-Cabau reports financial relationships with Edwards Life Sciences and Medtronic and holds the research chair “Fondation Famille Jacques Lariviere” for the Development of Structural Heart Disease Interventions. Otto reports no relevant financial relationships.
JACC Cardiovasc Interv. Published online November 8, 2021. Abstract, Editorial
For more news, follow Medscape on Facebook, Twitter, Instagram, and YouTube.
Source: Read Full Article