Romosozumab May Not Increase Cardiovascular Risk After All
The potent anabolic, antiosteoporosis agent romosozumab has been saddled with an Food and Drug Administration–mandated black-box warning for increased cardiovascular risk that may not be warranted, Glenn Haugeberg, MD, PhD, asserted at the 2021 Rheumatology Winter Clinical Symposium.
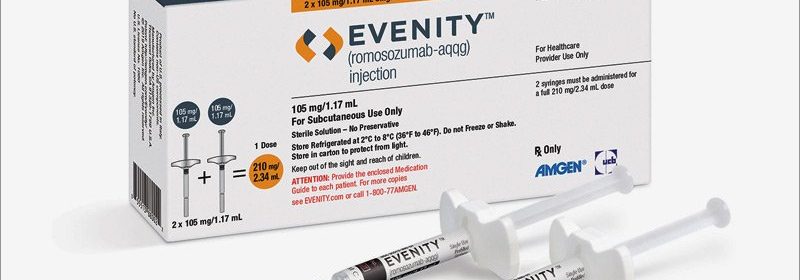
The black-box warning states that romosozumab (Evenity), a monoclonal antibody approved in 2019 for fracture prevention in patients with osteoporosis, may increase the risk of MI, stroke, and cardiovascular death. The warning arose from FDA concerns raised by the results of the phase 3 ARCH trial in which 4,093 postmenopausal women at high fracture risk were randomized to monthly subcutaneous injections of romosozumab or weekly dosing of the oral bisphosphonate alendronate (Fosamax) for 1 year, followed by 12 months of open-label alendronate for all. Alarm bells went off at the FDA because during year 1, the incidence of adjudicated major adverse cardiovascular events was 2.5% in the romosozumab arm, compared with 1.9% with alendronate.
Could a Cardioprotective Effect of Bisphosphonates Explain Cardiovascular Concerns?
However, evidence from multiple animal and human studies suggests that bisphosphonates actually have a cardioprotective effect. For example, a Taiwanese population-based cohort study of 1,548 patients on bisphosphonate therapy for osteoporotic fractures and 4,644 individuals with hip or vertebral fractures who were not on a bisphosphonate showed a 65% reduction in the risk of acute MI during 2 years of follow-up in those who received a bisphosphonate.
“That may explain the ARCH finding. It may – I say may – be that this concern in the ARCH study can be explained by the positive effect of the bisphosphonates on cardiovascular events,” according to Haugeberg, head of the division of rheumatology at the Southern Norway Hospital Trust, Kristiansand, and professor of medicine at the Norwegian University of Science and Technology, Trondheim.
He noted that, in the FRAME trial, another pivotal phase 3 trial of romosozumab, there was no signal of increased cardiovascular risk, compared with placebo. In FRAME, which included 7,180 osteoporotic postmenopausal women, rates of major adverse cardiovascular events and other adverse events were balanced between the two study arms at 12 months. Indeed, the incidence of adjudicated serious cardiovascular events was 0.5% with romosozumab and 0.4% with placebo injections. After 12 months, all participants were transitioned to denosumab (Prolia) for another 12 months. At 24 months, there remained no significant between-group difference in cardiovascular events, cancer, osteoarthritis, hyperostosis, or other major adverse events.
Potency of Romosozumab
Romosozumab’s efficacy for fracture prevention in these two pivotal trials was striking. The risk of new vertebral fractures was reduced by 73% with romosozumab, compared with placebo at 12 months in FRAME, and by 75% at 24 months in the romosozumab-to-denosumab group.
“FRAME was a 12-month study for the primary endpoint. The bisphosphonate studies typically had a 3-year design in order to show benefit, but here you see only 12-month follow-up. This illustrates the potency of this drug. We saw rapid increase in bone density and a huge decrease in new vertebral fractures versus placebo in the first 12 months, then during follow-up with denosumab the reduction in fractures was maintained,” the rheumatologist commented.
In the ARCH trial, where romosozumab went head to head with a very effective oral bisphosphonate, the risk of new vertebral fractures was 48% lower at 24 months in the romosozumab-to-alendronate group than in women on alendronate for the full 24 months, while the risk of hip fractures was reduced by 38%.
Romosozumab is a humanized monoclonal antibody with a novel mechanism of anabolic action: This agent binds to sclerostin, which is produced in osteocytes. When sclerostin binds to receptors on osteoblasts it reduces their activity, thereby inhibiting bone formation. Romosozumab takes away this inhibition of osteoblasts, boosting their activity. The result is increased bone formation accompanied by decreased bone resorption. This allows for a logical treatment approach: first using an anabolic agent – in this instance, subcutaneously injected romosozumab at 210 mg once monthly for 12 months – then switching to an antiresorptive agent in order to maintain the gain in bone mineral density and decrease fracture risk. This is the same treatment strategy recommended when using the anabolic agents teriparatide (Forteo) and abaloparatide (Tymlos); however, those parathyroid hormone and parathyroid hormone–related protein analogs are seldom used in Norway because their cost is substantially greater than for romosozumab, he explained.
Updated Endocrine Society Guidelines
Haugeberg called romosozumab “a new and wonderful drug.” The Endocrine Society also considers romosozumab an important new drug, as evidenced by the release of an 8-page update of the group’s clinical practice guideline on the pharmacologic management of osteoporosis in postmenopausal women; the update was devoted specifically to the use of romosozumab. The update, published in response to the biologic’s recent approval by U.S., Canadian, and European regulatory agencies, came just 10 months after release of the Endocrine Society’s comprehensive 28-page clinical practice guideline.
Haugeberg is a fan of the Endocrine Society guideline, which recommends romosozumab as a first-line therapy in postmenopausal women at very high risk of osteoporotic fracture, defined as those with a history of multiple vertebral fractures or severe osteoporosis with a T score of –2.5 or less at the hip or spine plus fractures. The updated guideline also recommends consideration of the antisclerostin biologic in high-risk patients who have failed on antiresorptive treatments.
The practice guideline states that the issue of a possible cardioprotective effect of alendronate in the ARCH trial “remains uncertain at this time.”
“Women at high risk of cardiovascular disease and stroke should not be considered for romosozumab pending further studies on cardiovascular risk associated with this treatment,” according to the Endocrine Society.
Haugeberg reported receiving research grants from Pfizer and Biogen and serving as a consultant to and/or on speakers’ bureaus for Amgen, which markets romosozumab, and more than a dozen other pharmaceutical companies.
This article originally appeared on MDedge.com, part of the Medscape Professional Network.
Source: Read Full Article