Ophthalmologists Detail Eye Injuries From Huge Beirut Blast

On the evening of August 4, 2020, about 2700 tons of ammonium nitrate exploded at the Port of Beirut in Lebanon, creating a supersonic blast wave that killed more than 200 people, injured 6000 more, and left 300,000 citizens homeless. More than 400 ophthalmic injuries were reported across the city. Ten people developed functional blindness. Now, 1 year after the blast — one of the largest nonnuclear explosions in history — ophthalmologists are describing the type of eye injuries they encountered in the aftermath of the explosion.
“The resulting storm of debris and shrapnel from shattered glass windows and building facades was the main source of injury to most patients,” write Ramzi M. Alameddine, MD, an ophthalmologist at the American University of Beirut Medical Center (AUBMC), in Beirut, Lebanon, and colleagues in an article published on August 5 in JAMA Ophthalmology. This shrapnel caused deep periocular lacerations, facial scarring, and in a few cases, injuries that required enucleation or evisceration, the authors report.
For the study, researchers reviewed medical records from people with eye injuries resulting from the blast who sought care at AUBMC. All patients included in the study presented at the emergency department or one of 13 AUBMC ophthalmology outpatient clinics from August 4 through November 2020. In addition to types of ocular injuries, the researchers also report final best-corrected visual acuity and need for surgical intervention as main outcomes.
Thirty-nine patients sought care at AUBMC during the study period for eye injuries resulting from the blast. Twenty-two of them presented with ocular injuries on the day of the explosion; the remaining 17 received treatment at ophthalmology clinics before the end of November. The group included 35 adults and four pediatric patients; 24 (61.5%) were female. There were 48 eye injuries in total, the researchers report, accounting for bilateral injuries in nine patients.
A patient with a complex deep right brow and upper eyelid laceration.
The most common injuries were surface injuries (54.2%). These included injuries from glass and shrapnel as well as chemical injuries or abrasions. Patients also presented with eyelid lacerations (41.6%), orbital fractures (29.2%), brow lacerations (20.8%), and open globe injuries (20.8%). This high rate of globe injuries is “comparable with the Oklahoma City bombing (22%) and Texas ammonium nitrate blast (42.9%) that similarly occurred in close proximity to residential buildings,” the authors note.
External photograph of a patient 7 weeks after the explosion, with resulting extensive facial and periocular scars and left eye phthisis bulbi secondary to multiple globe lacerations.
Twenty-one patients needed surgical intervention; four patients underwent enucleation or evisceration. Seven injured eyes (14.5%) had final best-corrected visual acuity of <20/200, including the injuries that required eye removal.
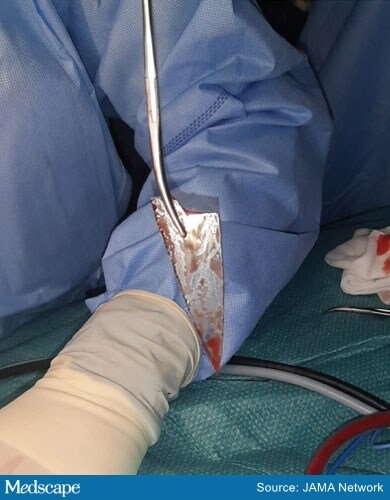
A large spear-like glass shard that was surgically extracted from a patient’s right orbit.
Although the study only focused on immediate outcomes, these patients with ophthalmic injuries “will require major long-term health care resources for years to come,” write Richard J. Blanch, MBChB, PhD, of the University Hospitals Birmingham NHS Foundation Trust, in Birmingham, United Kingdom, and colleagues in an invited commentary. “We also know that if blast-associated open globe injuries receive only initial repair without vitreoretinal surgical reconstruction, then around 50% of patients develop severe proliferative vitreoretinopathy,” they write. They point out that subsequent access to high-quality care is often necessary for secondary retinal procedures.
The report highlights the importance of triaging eye care in emergency situations. “Ophthalmic injury falls out of some triage tools, with patients with isolated eye injuries being classified as the walking wounded,” they write. The authors note that on the day of the blast, mild injuries were turned away. It was not clear whether any of the 17 patients who sought care at outpatient clinics were originally turned away from the emergency department on the day of the blast. If so, that may have affected patient outcomes.
A triaging system that moves lower-priority patients to care facilities farther away might solve both the patient and healthcare personnel problems in emergency situations, Blanch and colleagues note. “Well-constructed ocular trauma systems can run both ways for the benefit of all,” they write, “with less severe injuries being sent down the echelon to appropriate capable smaller units when higher-order facilities themselves are overwhelmed.”
The authors have disclosed no relevant financial relationships. Blanch is a serving member of the British Armed Forces.
JAMA Ophthalmology. Published August 5, 2021.
For more news, follow Medscape on Facebook, Twitter, Instagram, and YouTube.
Source: Read Full Article