A Technique for Measuring Brain Cell Injury in TBI
The study covered in this summary was published on medRxiv.org as a preprint and has not yet been peer reviewed.
Key Takeaway
-
An automated tractography pipeline with diffusion MRI tractography is helpful for identifying and quantifying traumatic axonal injury in the acute phase of severe traumatic brain injury.
Why This Matters
-
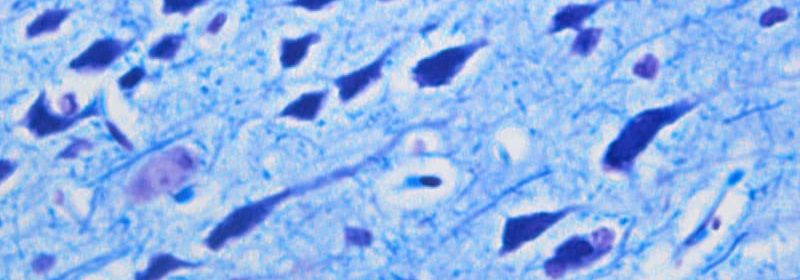
Traumatic axonal injury is the most common consequence of head trauma and is associated with adverse clinical outcomes.
-
Using this process to complement conventional MRI can aid in predicting outcomes and guiding decision-making regarding treatment in the intensive care unit and rehabilitation after the acute care.
Study Design
-
This was a prospective study on 18 patients aged 18-65 years with acute severe traumatic brain injury.
-
The patients had traumatic comas (Glasgow Coma Scale total score of 6 and no eye opening for 24 hours after their injuries).
-
The patients were compared to 33 healthy controls of approximately the same ages.
-
Right before each patient’s MRI, their level of consciousness (LOC) was assessed by a neurologist using the Glasgow Coma Scale, the Coma Recovery Scale-Revised, and the Confusion Assessment Protocol.
-
Neurologic exams and Glasgow Coma Scale assessments were done every 2-4 hours.
-
Once the patients were stable for transport, MRIs were performed and diffusion-weighted imaging data were obtained.
-
The images were corrected for distortions and movement.
-
The tractography algorithm TRACULA (TRActs Constrained by UnderLying Anatomy) was used for automated reconstruction of 40 major white matter pathways.
-
Metrics for each reconstructed tract were used to do a pointwise assessment of the tractography attributes.
-
Using TRACULA, each anatomical segmentation was converted to the subject’s individual diffusion MRI space.
-
A qualitative evaluation was done to look at how accurate the tract reconstructions were in the patients with severe TBIs.
-
The feasibility of performing TRACULA in a clinical setting needed more than 50% of the automated reconstructions to be successful. They were considered successful if the tracts crossed the white matter regions and reached the cortical areas used to define those tracts. For focal lesions, they were considered successful if the tract got to the cortical termination regions even if they had to go around the lesion.
-
Any failed or partial reconstructions were re-run.
-
For each patient, the extent of the traumatic axonal injury was measured using a multivariate analysis that incorporated along-tract measures of both fractional anisotropy and mean diffusivity.
-
The pipeline’s ability to discriminate between patients and controls was computed in order to assess the accuracy of detecting the traumatic axonal injury.
-
The effect of head motion was calculated for each patient with a total motion index.
-
Regression analyses were done to test the behavioral measures’ relationships.
Key Results
-
Tracts were successfully constructed by the TRACULA pipeline in 93% of the tracts (even when there were large focal lesions), which was 43% more than needed for this process to be feasible.
-
Multivariate individualized assessment of white matter damage was performed and showed that in patients with a TBI, 9.07 (standard deviation ± 7.9) tracts were abnormal.
-
The multivariate analysis found at least 1 abnormal tract in the white matter in each patient with a TBI; the most affected areas were the premotor, parietal, and temporal sections of the corpus callosum.
-
Patients and healthy controls were accurately differentiated from each other.
-
Head motion was found to not be a significant factor in detecting affected tracts (patients vs controls, P = .05)
-
The average Mahalanobis distance of affected tracts was not significantly correlated with Glasgow Coma Scale-Total (P = .55), Coma Recovery Scale-Revised Total (P = .65), days to command-following (P = .27), or days in coma (P = 1.00).
-
The number of affected tracts was also not significantly associated with Glasgow Coma Scale-Total (P = .26), Coma Recovery Scale-Revised Total (P = .19), days to command-following (P = .65), or days in coma (P = .56).
-
Additionally, there were no significant associations between the average Mahalanobis distance of affected tracts and level of consciousness (P = .136) or the number of affected tracts and LOC (P = .582).
Limitations
-
There are additional clinical factors besides traumatic axonal injury that can affect LOC of patients in the intensive care unit and could have affected the relationship with the behavioral measures of consciousness.
-
Disruptions in the brainstem that are not reconstructed by TRACULA may have also affected the associations with the behavioral measures of consciousness.
-
The sample size (small) and the difference in number of days before an MRI was performed could have underpowered the analysis.
-
The extensive focal lesions in several patients limited reconstruction of some tracts.
Disclosures
-
This study was supported by the US Department of Defense, NIH National Institute of Neurological Disorders and Stroke, NIH Director’s Office, NIH National Institute of Biomedical Imaging and Bioengineering, NIH National Institute of Mental Health, James S. McDonnell Foundation, American Academy of Neurology, Tiny Blue Dot Foundation, the Administration for Community Living, and the National Institute on Disability, Independent Living and Rehabilitation Research.
-
The authors report no relevant disclosures.
This is a summary of a preprint research study, “Automated detection of axonal damage along white matter tracts in acute severe traumatic brain injury,” written by Chiara Maffei, PhD, from the Martinos Center for Biomedical Imaging, Massachusetts General Hospital and Harvard Medical School, Charlestown and the Center for Neurotechnology and Neurorecovery, Department of Neurology, Mass General, Boston, and colleagues, on MedRxiv, provided to you by Medscape. This study has not yet been peer reviewed. The full text of the study can be found on medRxiv.org.
For more news, follow Medscape on Facebook, Twitter, Instagram, YouTube, and LinkedIn
Source: Read Full Article