Protein based biomarker identifies chemo drug sensitivity
Cancer is one of the world’s second deadliest disease which contributes to the death of over 10 million people per year. Oncologists adopt a variety of treatment procedures to treat cancer cells. Among the different methods used to fight cancer, chemotherapeutic treatment is a prominent and well-adopted technique. It is a drug based method, wherein powerful chemical compounds are injected into the body to annihilate the malignant cells. Although these chemicals support the destruction of the cancerous cells, optimizing their dosage has always been a challenge to the medical specialists.
Cisplatin is a chemotherapy medication which is used to treat a number of cancers such as lung cancer, brain tumor, breast cancer, liver cancer etc. This platinum-metal based chemotherapy drug is highly powerful and is instituted by the intravenous route into the body. Although it is renowned for effective destruction of cancerous cells for the past 4 decades, its alarming side effects is of serious concern to the medical community. Researchers have reported that administration of high dosage of the chemical is not only ineffective on the tumor cells but is also responsible for adverse side effects which may even lead to the sudden demise of the patient. The control on the level of the cisplatin drug has been a matter of persisting concern for medical practitioners.
A recent study on monitoring the cisplatin level in liver cancer cells reported by researchers from the Graduate School of Medical and Dental Sciences at Niigata University, Japan and their collaborators from Niigata Medical Center, Uonuma Institute of Community Medicine Niigata University Hospital, Niigata City General Hospital, Saiseikai Niigata Hospital and, Kashiwazaki General Hospital and Medical Center provides a ray of hope to the health professionals.
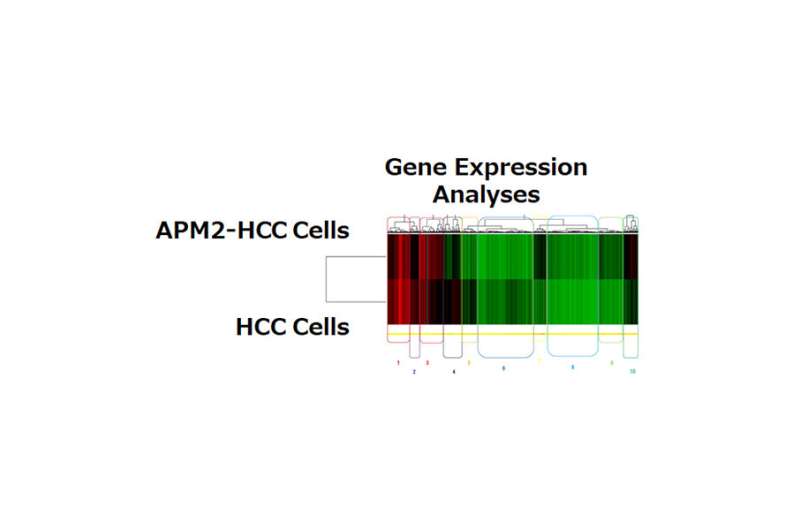
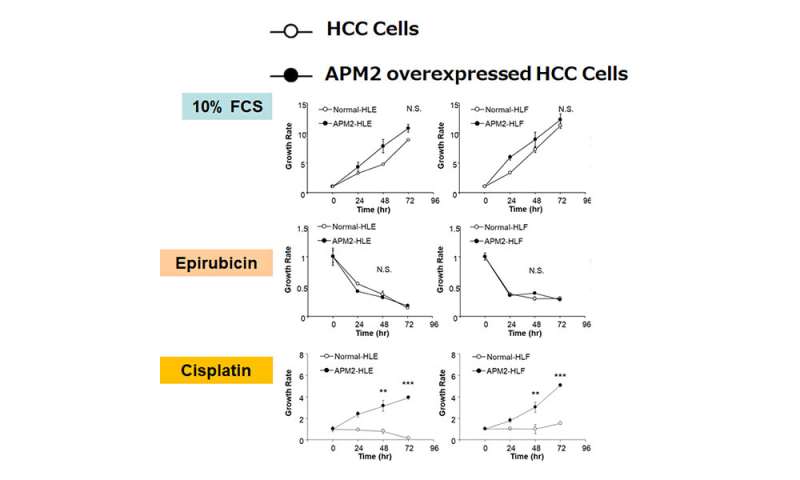
The findings were published recently in the prestigious Scientific Reports journal from Nature. The multi-disciplinary research team has identified adipose most abundant 2 protein (APM2) as a potential marker to indicate the permissible level of the drug. They have experimentally investigated the liver and gastro cancer cells and have compared the variation in the protein concentration in the presence and absence of the chemo drug.
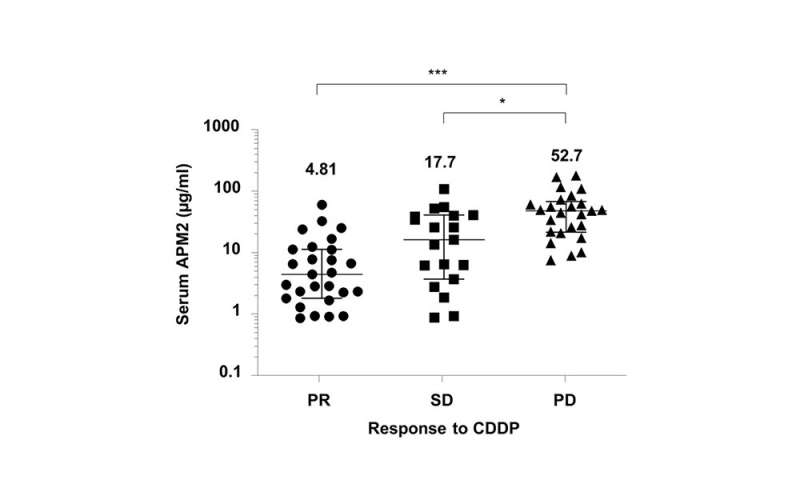
“Our results demonstrate a significant relationship between the high level of APM2 expression in serum, cancerous cells in the liver, the surrounding liver tissue and cisplatin resistance. The study reveals that APM2 expression is related to cisplatin sensitivity” explains Professor Kenya Kamimura of the Division of Gastroenterology and Hepatology, the Graduate School of Medical and Dental Sciences, Niigata University. The research study paves way for effective monitoring of chemotherapeutic drug level and their safe administration. Professor Kenya Kamimura states with confidence that, “The serum APM2 can be an effective biomarker of the liver and gastric cancer cells for determining the sensitivity to cisplatin. The results of the study would provide an advantage for the technicians, allowing easy adaption in small local clinics.”
The research group has noticed that APM2 concentration favors the development of the ERCC6L gene card. This is manifested by the growth of the cancerous cells and marks the resistance to the chemo drug. The valuable findings offer the potential to control the cisplatin dosage level and avoid cytotoxicity. Such a study is essential in today’s context as research groups across the globe strive to develop new methodologies to optimize the dosage and control the severe side-effects induced by the concentration of chemo drugs. The research team has also utilized bioinformatics based tools to complement the experimentally obtained results.
“To the best of our knowledge, this is the first report to demonstrate that the serum level of APM2 can be the predictor of CDDP chemosensitivity. This study thus represents a milestone for detecting CDDP sensitivity, and further studies will help modify APM2 expression, which could contribute to the chemosensitization of the tumor,” describes Professor Kenya Kamimura.
Source: Read Full Article