Triple negative breast cancers can adopt reversible state that is resistant to chemotherapy
Researchers at The University of Texas MD Anderson Cancer Center have discovered that triple negative breast cancer (TNBC) cells can develop resistance to frontline, or neoadjuvant, chemotherapy not by acquiring permanent adaptations, but rather transiently turning on molecular pathways that protect the cells.
The study, published today in Science Translational Medicine, also identifies a vulnerability that may provide a new treatment option for resistant TNBC. Among those pathways activated is a metabolic process, known as oxidative phosphorylation, which can be targeted by a small-molecule drug developed by MD Anderson’s Therapeutics Discovery division.
“Modern chemotherapy is highly effective for nearly half of patients with triple negative breast cancers,” said corresponding author Helen Piwnica-Worms, Ph.D., professor of Experimental Radiation Oncology. “However, the remaining half of women will not fully respond to neoadjuvant chemotherapy, and there currently are no approved treatments to improve outcomes for them. Understanding how tumor cells become resistant will allow us to identify new targets to better treat resistant disease.”
According to the American Cancer Society, an estimated 268,000 women will be diagnosed with breast cancer this year, of which 15 to 20 percent will have TNBC. Standard treatment for patients with TNBC is neoadjuvant chemotherapy followed by surgery to remove the tumor. For women with tumors that don’t fully respond to chemotherapy, there is a much higher risk of recurrence and death from the disease, said Piwnica-Worms.
In order to study how TNBC cells become resistant to treatment, the researchers created mouse models, known as patient-derived xenografts (PDXs), of TNBC using tumor samples from patients enrolled in the ARTEMIS clinical trial, led by MD Anderson’s Breast Cancer Moon Shot.
Patients enrolling in ARTEMIS have tumor biopsies taken before and after neoadjuvant chemotherapy treatment, which enable researchers to study why some tumors are resistant and discover more effective strategies to bring cures to more patients. The work is part of MD Anderson’s Moon Shots Program, a collaborative effort designed to accelerate the development of scientific discoveries into clinical advances that save patients’ lives.
Piwnica-Worms’ team identified several PDX models that responded to chemotherapy at first, but eventually developed resistance and resumed tumor growth. If treatment was paused, however, the residual tumors once again became sensitive to chemotherapy, indicating the resistance was temporary.
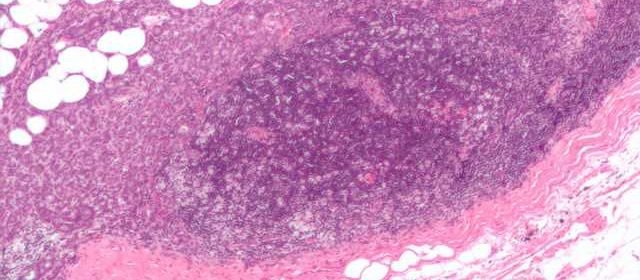
Under the microscope, tumors showed distinct changes during treatment, but regrown tumors appeared similar to those before treatment. Further, an analysis of individual tumor cells showed that the heterogeneity of cells in a given tumor was maintained after treatment, suggesting that chemotherapy did not select for a small subset of resistant cells.
Characterization of gene expression changes revealed a set of pathways activated as part of the resistant state, which were turned off when chemotherapy was discontinued. The researchers confirmed many of these molecular changes were mirrored in biopsies taken from ARTEMIS patients.
Hoping to find new treatment targets for resistant TNBC, the researchers discovered that these cells had become dependent on oxidative phosphorylation for energy production. This pathway is the target of IACS-10759, the first-small molecular discovered and developed by MD Anderson’s Therapeutics Discovery division.
When treating the PDX mice with IACS-10759 following chemotherapy treatment, the researchers observed a synergistic effect, suggesting sequential treatment of chemotherapy and IACS-10759 could prolong the duration of treatment response. IACS-10579 is now in clinical trials for a variety of hematological and solid cancer types.
Source: Read Full Article
