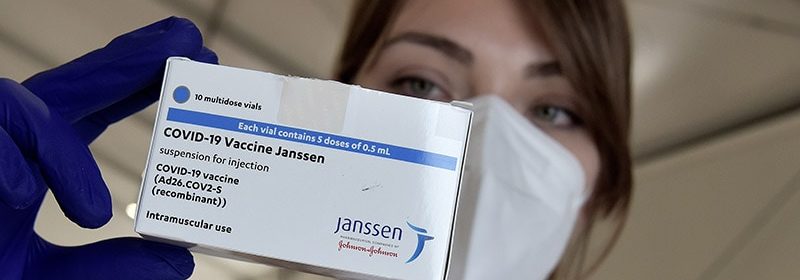
Restrict J&J COVID Vaccine in Women Under 50?
Editor’s note: Find the latest COVID-19 news and guidance in Medscape’s Coronavirus Resource Center.
Use of mRNA COVID-19 vaccines should be considered as the preferable option in the US rather than Johnson & Johnson’s (J&J) Janssen COVID-19 vaccine in women under the age of 50 years, according to one group of experts.
The group makes their recommendation in an editorial in JAMA published online April 30, accompanying a paper describing details of 12 case reports of cerebral venous sinus thrombosis (CVST) with thrombocytopenia following the J&J COVID-19 vaccine, also known as the Ad26.COV2.S vaccine.
The editorialists are Ruth A. Karron, MD, professor of international health at Johns Hopkins Bloomberg School of Public Health in Baltimore, Maryland; Nigel S. Key, MD, professor of hematology at University of North Carolina at Chapel Hill; and Joshua M. Sharfstein, MD, associate dean for public health practice at Johns Hopkins Bloomberg School of Public Health.
They note that after an initial pause following reports of thrombosis with thrombocytopenia syndrome (TTS) linked to the J&J vaccine, and on the recommendation of the Advisory Committee on Immunization Practices, the US has permitted the use of the J&J vaccine in all adults with information on the risk of TTS added to educational materials.
The editorialists point out that no cases of TTS have been confirmed following administration of more than 180 million doses of the mRNA vaccines in the US.
They say that while the J&J vaccine will still be needed for individuals with allergies to components of the mRNA vaccines and for those who live in remote locations where the cold chain for transport and storage of mRNA vaccines cannot be maintained, “US public health agencies and clinicians should consider recommending mRNA vaccines as safer options for those who may be at substantially higher risk for TTS after Ad26.COV2.S vaccination, currently women younger than 50 years.”
In the main JAMA paper, a group led by Isaac See, MD, Centers for Disease Control and Prevention (CDC) COVID-19 Response Team, report full details of 12 cases of CVST with thrombocytopenia following the J&J COVID-19 vaccine reported to the US Vaccine Adverse Event Reporting System (VAERS).
The 12 US case reports, three of which were fatal, show many similarities to cases described in Europe after the AstraZeneca vaccine.
The authors note that by April 12, approximately 7 million doses of the J&J vaccine had been given in the US. The 12 cases of CVST and thrombocytopenia following receipt of the vaccine were reported to VAERS between March 2 and April 21. All 12 cases were in white women, 11 of whom were under 50 years of age.
As of April 25, a further two cases have been confirmed and reported to VAERS; one in a man younger than 40 years, the other in a woman aged between 40 and 59 years.
In the 12 cases reported in detail, symptoms started between 6 and 15 days post vaccination.
At least 1 risk factor for CVST was identified in 7 patients (obesity in 6, hypothyroidism in 1, and use of combined oral contraceptives in 1). None of the patients was pregnant or within 12 weeks postpartum, had prior thrombosis, a personal or family history of thrombophilia, or documented prior exposure to heparin.
In addition to CVST, seven patients had intracerebral hemorrhage and eight had non-CVST thromboses.
One patient reported a history of SARS-CoV-2 infection approximately 4 months prior to vaccination. Of the other 11 patients, four had negative serologic tests and seven were not tested.
All 12 patients were hospitalized and 10 were admitted to an intensive care unit (ICU). At the time of the last follow-up, three patients had died (all of whom had intraparenchymal hemorrhage), three remained in the ICU, two were still hospitalized but not in an ICU, and four had been discharged home.
The authors point out that the US cases of CVST with thrombocytopenia following the J&J vaccine have many similarities to those reported in Europe after the AstraZeneca vaccine, occurring primarily in women younger than 40 years and in patients without diagnosed thrombophilia. Both European and US patients had a median platelet nadir count of 19×103/µL and several also had non-CVST large-vessel thrombosis.
In the European cases of CVST with thrombocytopenia, 50% of patients died, compared with 25% of US patients.
Like the European cases, the US cases had positive heparin-PF4 HIT antibody ELISA tests in the absence of prior exposure to heparin, as would be seen in autoimmune HIT.
However, in the initial European CVST reports, 88% of patients tested with functional platelet HIT antibody tests had positive results, compared with only 11% of the US cases. But the authors note that lack of standardization in functional platelet HIT antibody assays may lead to differences in results by different laboratories.
“It may be important to notify testing laboratories that post-vaccination TTS is being evaluated, so that testing methods can be adjusted if needed,” they say.
They conclude that these case reports suggest that the pathogenesis of TTS may be similar to autoimmune HIT, triggered by the formation of antibodies directed against PF4, a constituent of platelet alpha granules released during platelet activation. In contrast to classic HIT in which exogenous heparin triggers antibody formation, in autoimmune HIT, an endogenous polyanion triggers PF4 antibody formation.
They note that the precise mechanism of TTS in relation to COVID-19 vaccination has not yet been established. The Global Advisory Committee on Vaccine Safety has stated that a platform-specific mechanism related to adenovirus vector vaccines cannot be excluded. Both the J&J and AstraZeneca vaccines use an adenoviral vector, but they are different; J&J uses a human vector, while AstraZeneca uses a chimpanzee vector.
They also point out that CVST and thrombocytopenia following SARS-CoV-2 infection has been reported in at least two cases, but HIT testing was not done in these cases. There have not so far been any reports to VAERS of CVST with thrombocytopenia following mRNA COVID-19 vaccines.
The authors say these findings have important clinical and public health implications, noting that the CDC has updated its interim clinical considerations for use of authorized COVID-19 vaccines to indicate that women aged 18 to 49 years should be aware of the increased risk of TTS after receipt of the J&J vaccine, and to use a nonheparin anticoagulant in suspected cases.
They note that a subacute presentation of headache is present in 90% of patients with typical CVST. While headache is a common symptom after the J&J vaccination, most headaches begin and resolve within two days. Whereas in the US cases of CVST after vaccination, headache symptoms began at least six days after vaccination and persisted for at least a week for most.
“Urgent consultation with a neurologist is prudent when a patient is suspected or confirmed to have CVST. In addition, since the median time from symptom onset to hospitalization was seven days in the US CVST case series, patient and clinician education might shorten the time to clinical evaluation and therefore treatment,” they state.
The authors also note that VAERS is a passive surveillance system, so cases of CVST with thrombocytopenia may be underreported.
In their accompanying editorial, Karron et al point out that in addition to the 12 patients with CVST with thrombocytopenia described in this case series, at least three patients without CVST but meeting diagnostic criteria for TTS have been reported to VAERS (as of April 21), all in women aged 18 to 59 years (median age, 37 years).
The editorialists report that the rate of CVST with thrombocytopenia after the J&J vaccine is approximately 5 per million women aged 18 to 50 years. This is compared with a background rate of approximately 0.05 to 0.13 per million per month.
They say that the availability of an interim standardized case definition of this adverse effect will facilitate prospective case ascertainment through review of large linked databases and active case finding.
This will also permit greater understanding of whether individuals who are otherwise at increased risk for hypercoagulation in general and for CVST in particular (for example, women taking hormonal contraceptive medications or who are pregnant) are also at increased risk for TTS.
Obtaining this information will support dynamic country-specific assessments of the risks of each vaccine compared with the risk of COVID-19 disease for their populations and subpopulations, they add.
JAMA. Published online April 30, 2021. Full text, Editorial
For more Medscape Neurology news, join us on Facebook and Twitter.
Source: Read Full Article