Microbiologists’ work adds to research on microbiome fungi and childhood disease

A surge in research projects on the human microbiome—the complex ecosystem of microorganisms in the human gastrointestinal tract—is bolstering scientific understanding of health, disease and environment. Much of the research has focused on gut bacteria and viruses, leaving a third factor—fungi—little studied.
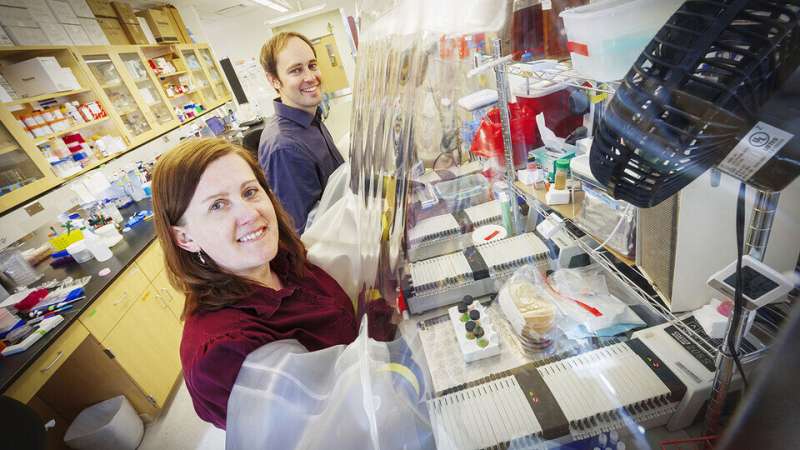
An international consortium of scientists has conducted the first large-scale study of gastrointestinal fungi throughout early childhood. The research team included Thomas and Jennifer Auchtung, husband and wife microbiologists in the University of Nebraska–Lincoln’s Food Science and Technology Department.
The findings, recently published in the journal Nature Communications, help fill significant gaps in scientific knowledge of the fungal dimensions of the microbiome and identify areas for further study.
“Gut microbe interactions in early childhood are critical for proper immune responses,” the study said, “yet there is little known about the development of the fungal population from infancy into childhood.”
To look for answers, six clinical research centers participated, studying stool samples of 888 children ages three months to 48 months from Washington, Colorado, Georgia and Florida, as well as Germany, Sweden and Finland. The research particularly focused on possible connections between gastrointestinal fungi and the occurrence of Type 1 diabetes. Previous studies suggested that individuals with the disease have atypical gastrointestinal fungal communities. This new study—part of a project that goes by TEDDY, or The Environmental Determinants of Diabetes in the Young—collected samples from children before they developed disease and thus allowed researchers to address what may be causing illness.
Because there are many questions about fungi and other factors that could contribute to the development of autoimmune diseases such as Type 1 diabetes and celiac disease, the TEDDY project assembled this major data sample of international scope to help provide answers. Nebraska’s Holland Computing Center was a key resource, providing the analytical power to process the collected information.
Completion of the project’s fungal research was headed by Thomas Auchtung, an adjunct professor of food science and technology and research scientist and lab manager for Synbiotic Health, a microbiology company whose founders include several Husker faculty members. Synbiotic Health is based at Nebraska Innovation Campus.
The wide-ranging analysis by the TEDDY researchers did not find a strong association between gut fungi and the children who developed Type 1 diabetes. But, “there was a species of fungi that was more common in children who later developed celiac disease,” Thomas Auchtung said. Celiac disease is an autoimmune disorder of the small intestine.
That fungal species is Candida sake. “Children later diagnosed with celiac disease,” the study reported, “were found to have an increased abundance of Candida sake after six months.” Little has been published about fungi in celiac disease patients and “these findings show the need for follow-up studies,” said Jennifer Auchtung, assistant professor of food science and technology. Such research “could look to see if this was a correlation or if there are more substantive, causative relationships between this species of fungi and those who go on to develop celiac disease later in life.”
Understanding fungal populations in the human gastrointestinal tract is important overall.
“There is some debate whether fungi are resident members of the gut or are transient members mostly coming from the foods we eat,” Thomas Auchtung said.
Fungi play important roles in producing fermented foods such as bread, wine and beer. While the fungi in these foods are often removed or inactivated prior to consumption, live fungi can be consumed through fermented foods that contain live and active microbes, such as some types of beer, kombucha and blue cheese. There is even a fungal probiotic, Saccharomyces boulardii.
“Because of these many opportunities for fungi to be present in our gut, further research is needed to better understand how fungi might contribute to health and disease,” Jennifer Auchtung said.
Additional findings from the TEDDY study:
- Lack of a stable fungal community; more information needed on anti-fungal immunity. The researchers reported that “in young children, despite increased episodes of sickness and the presence of an immature bacterial community, there was no indication of a stable fungal community, or ‘mycobiome,” inhabiting the gut. Nevertheless, even nonviable and non-metabolically active fungi and their cellular components can provoke an immune response, so differences in fungal exposures at a young age may have immediate and lasting immunological impacts.”
- The study stated that “having proper fungal exposures may be crucial for children to establish appropriate responses to fungi and limit the risk of infection. The data here suggests those gastrointestinal exposures are limited and variable.” Follow-up research can look “to establish the source of the many fungi that are detected in the gut, in order to understand variations in anti-fungal immunity and limit fungal exposures that increase risk of disease.”
- Lower overall fungal presence in young children than expected. “One thing researchers thought going in,” Thomas Auchtung said, “was that because children have an immune system that is not as well-developed, fungi might be more abundant. But instead, we found that fungi were even less common when children were young, counter to what was expected.”
- A difference from microbiome bacteria. The TEDDY research “has shown that fungi have a very different relationship with the developing infant gut than bacteria,” the study said. “The abundance and composition of fungal species changed with the transition from milk/formula to solid foods, but fungal diversity remained consistent,” in contrast to the bacterial trend.
Source: Read Full Article