Gut microbiota: How does it interact with the brain?
Through studies in mice, researchers find evidence that having a healthful balance of gut microorganisms is important for good health.
Researchers from the Institut Pasteur, French National Center for Scientific Research (CNRS), and Inserm have found evidence that gut microbiota also plays a role in mood regulation and brain function.
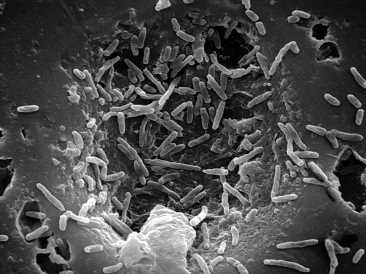
Gut microbiota is the community of bacteria, fungi, and viruses that live in the digestive tract.
These findings in mice suggest that changes to gut bacterial communities may lead or contribute to depression. If humans have a similar mechanism, doctors might be able to use bacteria strains to treat mood disorders, such as depression.
A group of 16 researchers from several prominent French research institutions conducted the study, which appears in Nature Communications.
Gut microbiota and mood
Studies have found that some people with depression experience dysbiosis, which is an imbalance or change in their intestinal microbiota.
Research conducted on rodents also shows that gut dysbiosis has associations with neurological changes linked with depression, such as:
- reduced adult neurogenesis, or the growth of new brain cells
- chronic low-grade inflammation
- abnormal hypothalamic–pituitary–adrenal (HPA) axis (the body’s central stress response system) function
Animal studies also show that gut microbiota helps regulate anxiety. It may also influence the development of neurological conditions caused by circuit dysfunctions, such as Parkinson’s disease, Alzheimer’s disease, depression, and obsessive-compulsive disorder.
Researchers think this is because gut bacteria release metabolites, tiny bits of food broken down by digestion that influence brain function. Metabolites may impact mood regulation by acting on the endocannabinoid system.
The endocannabinoid system is a complex cell-signaling system consisting of lipid (fat)-based neurotransmitters and their receptors.
It is found throughout the body and plays a role in important aspects of health, such as immune and nervous system function and cellular communication in the nervous system. It also regulates emotions, moods, and stress responses by activation of the system’s main receptor, CB1.
Previous research supports the idea that restoring gut microbial health may help treat depression. In animal studies, prebiotic treatment influenced emotional behavior. In human studies, prebiotic supplementation also improved mood in people with depression.
But despite educated theories, researchers still do not know precisely how gut bacteria impact brain function.
Researchers in the recent study set out to find the mechanisms linking gut microbiota and mood disorders. A team of researchers from some of these same French institutions published a report earlier this year, which found that stress-induced changes in gut microbiota reduced the efficacy of the antidepressant fluoxetine in mice.
The study
In the study, researchers submitted genetically identical mice to unpredictable chronic mild stress (UCMS), a mouse model of stress-induced depression, for 8 weeks.
This treatment caused the mice to develop depressive-like behaviors, such as reduced eating, grooming, weight loss, and hippocampal neurogenesis. The hippocampus is responsible for learning and memory and is heavily affected by several psychiatric and neurological conditions.
Researchers then transplanted fecal samples containing gut microbiota from control and UCMS-exposed mice into healthy mice. To serve as a control, mice that received fecal transplants were germ-free mice or received treatment with antibiotics for 6 days.
After 8 weeks, mice that received transplants from UCMS mice developed depression-like symptoms. The mice also experienced a reduction in the number of new brain stem cells and neurons in their hippocampus.
These findings show that transferring gut microbiota from stress-induced depressive mice to healthy mice induced depression-like behaviors.
“Surprisingly, simply transferring the microbiota from an animal with mood disorders to an animal in good health was enough to bring about biochemical changes and confer depressive-like behaviors in the latter.”
– Pierre-Marie Lledo, head of the Perception and Memory Unit at the Institut Pasteur (CNRS/Institut Pasteur), joint last author of the study
To figure out how this occurred, researchers explored the possibility that UCMS-exposed microbiota may trigger depression by altering metabolism. They found that mice with UCMS microbiota had significantly reduced levels of certain fatty acids in their blood and brain.
The reduced fatty acids included monoacylglycerols (MAG), diacylglycerols (DAG), polyunsaturated fatty acid (PUFA), and linoleic acid. monoacylglycerols (MAG), diacylglycerols (DAG), polyunsaturated fatty acid (PUFA), and linoleic acid. Variations of two of these fatty acids, DAD and PUFA, are converted into endocannabinoids (eCB).
The researchers speculate that gut dysbiosis may cause these changes in fatty acid levels. Studies link the dysregulation of the endocannabinoid system and its central receptor, CB1, with depression in both UCMS-model mice and humans.
In the study, the researchers found that mice with UCMS microbiota had greatly reduced levels of eCBs in their hippocampus and blood. They also found that mice with UCMS microbiota had reduced levels of Lactobacillus bacteria.
The researchers were able to reduce the depressive impact of the UCMS microbiota by enhancing CB1 levels and giving the mice a strain of Lactobacillus bacteria orally.
These findings suggest that chronic stress, diet, and the gut microbiota contribute to the development of depression-like behaviors via the endocannabinoid system.
“This discovery shows the role played by the gut microbiota in normal brain function,” says Gérard Eberl, Head of the Microenvironment and Immunity Unit (Institut Pasteur/Inserm) and joint last author of the study.
More specifically, imbalances in the gut bacterial community that reduce fatty acid levels vital to the endocannabinoid system and brain function seem to encourage the development of depression-like behaviors.
These findings mean certain bacteria could act as a natural antidepressant, treating mood disorders by restoring gut microbial health. And this is promising news, considering the slew of potential adverse side effects and relatively low efficacy rate of most current antidepressants.
To confirm their results, the researchers will need to test their findings in humans. The researchers say that new research will also need to explore whether changes to the gut microbiota impact other brain targets of the endocannabinoid system in the same way.
Source: Read Full Article
