Genes from tiny viruses can turn bacteria into superbugs
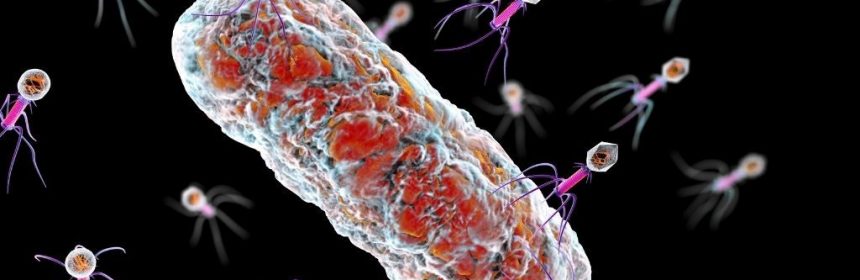
Viruses that infect bacteria may drive the evolution of drug-resistant superbugs by inserting their genes into the bacterial DNA, a new study suggests.
The bacteria-attacking viruses, called phages, act as parasites in that they depend on their hosts for survival. The viral parasites often kill off their microbial hosts after infiltrating their DNA, said senior study author Vaughn Cooper, director of the Center for Evolutionary Biology and Medicine at the University of Pittsburgh School of Medicine. But sometimes, the phages slip into the bacterial genome and then lay low, making sneaky changes to the bacterium’s behavior, Cooper said.
For instance, the virus may prompt the bacteria to secrete toxins that kill nearby phages, so the virus can keep its new host all to itself. But now, a new study, published Friday (July 16) in the journal Science Advances, hints that phages may also help their bacterial hosts develop resistance against antibiotic treatments.
In the new study, the team focused on Pseudomonas aeruginosa, a type of bacteria that ranks among the leading causes of hospital-acquired infections and is often resistant to multiple drugs. In particular, the bacterial infection often affects people with compromised immune systems, whether due to conditions like cystic fibrosis or drugs that suppress the immune system, like steroids.
Knowing that P. aeruginosa can be so difficult to kill, the team wondered how different strains of the microbe stack up against each other, and what makes the superior strains so good at triggering hard-to-treat infection. “If you have six different strains of Pseudomonas aeruginosa, who wins?” Cooper said.
The team tackled this question by introducing six different strains of P. aeruginosa into burn wounds on pigs. Soon enough, two of the six strains had completely taken over, driving the others to extinction. “That happened extremely quickly, within a couple of days,” Cooper said.
These two “winning” strains produced small, wrinkled-looking colonies of bacteria that congregated into biofilms — clusters of bacterial cells that secrete a slimy substance that offers them protection from both the host immune system and attacks by phages. The presence of biofilms and small, wrinkly cell colonies has been linked to slower wound healing and worse clinical outcomes, compared with infections that don’t bear these qualities, Cooper said.
In this case, the winning strains showed “hyperbiofilm formation,” far beyond any biofilm formation observed in the competing strains.
The biofilm slime protects the bacteria from the host immune system because immune cells struggle to glom onto the large matrix and gobble up the bacteria within. Phages also embed themselves in this protective matrix and release chemicals to fight off other phages in the neighborhood, again, to keep their bacterial hosts all to themselves.
What’s more, when bacteria begin producing biofilms, their metabolisms wind down and their cells divide more slowly; this can undermine the effects of antibiotic drugs, since many work by causing cells to short-circuit during cell division, Live Science previously reported.
The two winning strains of P. aeruginosa did not immediately produce biofilms upon entering the pigs, but instead entered this protectively slimy state as time progressed. To find out why, the team zoomed in on the winning strains’ DNA.
They compared the genetic sequence of the winning strains with their ancestors — the versions of those same strains that were first introduced to the pig wounds — to see whether any mutations had cropped up as the bacteria divided in the animals. They also compared the winning strains’ genetic sequences with those of the losing strains.
Instead of finding small mutations scattered throughout the DNA, the team found that entirely new segments of DNA had been added to the winning strains’ genomes. They identified these “foreign” bits of DNA as belonging to phages, those viruses that infect bacteria. And in fact, the phages in question first entered the pig wounds on the DNA of the losing bacteria strains.
In other words, once inside the wound, these phages leapt out of their original host bacteria and weaseled their way into the winning P. aeruginosa strains. In fact, cells sampled from the winning strains each had about one to four segments of new phage DNA added to their genetic codes.
Most notably, a phage inserted its genetic material into a gene called retS, an important switch that helps turn biofilm production on and off. When activated, retS acts as the off switch and suppresses biofilm production; but once the phage infiltrated this gene in the winning strains, retS could no longer be activated and biofilm production went wild.
—Medicine’s journey through the body: 4 stages
—Aspirin to Zoloft: The scoop on 5 medicines
—5 ways gut bacteria affect your health
The team stuck a normal version of retS back into the winning strains, to see if biofilm production would switch off again, and it did. This suggested that, yes, the phage-related changes in the gene had pushed the bacteria to produce biofilms and likely helped the winning strains dominate where the losing strains failed.
This finding hints that, early in the course of infections, phages might hop between bacterial strains, passing superpowers back and forth until one bug emerges victorious, and such as in this case, equipped with antibiotic-resistance. That said, it’s not clear how often people get infected with multiple strains of bacteria at one time, so there’s a question as to how often these sorts of swaps occur, Cooper said. In any case, the study hints that phages may play a key role in bacterial evolution and the rise of treatment-resistant bugs.
But phages aren’t all bad — the viruses could offer a clever strategy for taking down superbugs when all other treatments fail. Phages can kill bacteria by splitting the microbes open from the inside; the viruses do this after multiplying inside a bacterium, so when the bacterial cell splits, new copies of the phage spill out.
“With antibiotic resistance on the rise, the field has been interested in repurposing these viruses as antibiotics themselves,” Cooper said. To realize this ambition, scientists will need to better understand how phages infect their bacterial hosts and which phage genes help kill the hosts. And since a given phage usually infects only one species or strain of bacteria, developing phage-based drugs that work against many superbugs could present a challenge, he said.
“Most of the genes in phages are essentially dark matter to us,” so the field has a long way to go, Cooper said.
Originally published on Live Science.
Nicoletta Lanese is a staff writer for Live Science covering health and medicine, along with an assortment of biology, animal, environment and climate stories. She holds degrees in neuroscience and dance from the University of Florida and a graduate certificate in science communication from the University of California, Santa Cruz. Follow Nicoletta on Twitter @NicolettaML.
Source: Read Full Article