Carotid Surgery Still Too Risky With Contralateral Occlusion
Patients selected for carotid revascularization who have a contralateral carotid occlusion are still best triaged toward stenting rather than surgery, a new registry analysis suggests.
The study showed that contralateral carotid occlusion is an important predictor of risk for in-hospital death, myocardial infarction (MI), or stroke among patients undergoing carotid endarterectomy surgery, but not among those undergoing carotid artery stenting.
Dr Eric Secemsky
“This is one of the largest series of patients undergoing surgery or stenting for carotid stenosis who also have an occluded vessel on the other side,” senior author Eric A. Secemsky, MD, told Medscape Medical News.
“Carotid stenting has traditionally been the revascularization treatment of choice in this group, as surgery has been shown to be associated with an increased risk of stroke in the perioperative period in these patients. While recent observational studies have suggested that, with newer surgical techniques, the risk of surgery may now not be so great in these patients, our results strongly contradict that idea,” said Secemsky, who is director of vascular intervention at Beth Israel Deaconess Medical Center, Boston, Massachusetts.
“We found the increased risk of serious adverse outcomes with surgery is still there even in this contemporary era, and so stenting remains the preferred option in these patients,” he stated.
The study was published online in the Journal of the American College of Cardiology on February 15.
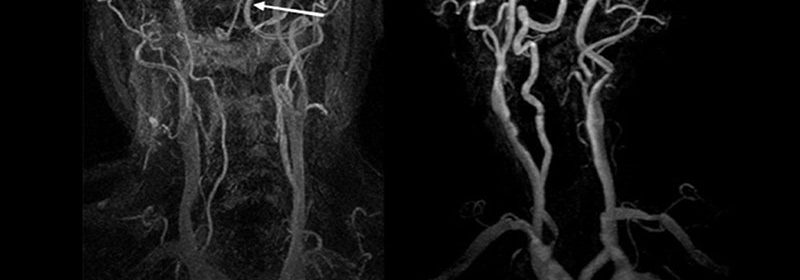
“If a patient has a fully occluded artery on one side, we generally don’t treat it. It isn’t considered to be a major risk for plaque breaking off and causing a stroke, so we normally just leave it alone,” Secemsky explained. “But if a patient is discovered to have a lesion on one side but a fully occluded artery on the other side, this puts them at higher risk for having the lesion treated.”
Approximately 8% to 10% of patients with carotid stenosis are found to have such a contralateral carotid occlusion.
Dr Anna Krawisz
Lead author Anna Krawisz, MD, chief cardiology fellow at Beth Israel Deaconess Medical Center, Boston, explained that carotid endarterectomy surgery requires clamping the artery, which can cause problems with hypoperfusion in patients with contralateral occlusion. “Stenting is much quicker and doesn’t cause a reduction in global blood flow to the brain, so has long been the revascularization strategy of choice for these patients,” she said.
Although earlier studies have shown higher stroke and death rates with surgery than stenting among patients with contralateral occlusion, newer observational data have called into question whether surgery is inferior to stenting among patients with contralateral occlusion in contemporary practice, the authors note. But they point out that patients referred for surgery are generally more robust than those who undergo stenting, and unmeasured confounding is always a problem in such comparisons.
To try to overcome this issue, the investigators employed a study that had a novel design. Rather than comparing stenting with surgery for patients with contralateral occlusion, they performed two comparisons: (1) stenting for patients with contralateral occlusion in comparison with stenting for patients without contralateral occlusion; and (2) surgery for patients with contralateral occlusion in comparison with surgery for patients without contralateral occlusion.
“In this way we are showing the risk associated with contralateral carotid occlusion for each procedure separately,” Secemsky commented.
“We found that in patients undergoing surgery, there was a much higher risk of death/MI/stroke in patients with a contralateral occlusion vs those without such an occlusion (a 71% increase in risk), but in those who underwent stenting, patients with a contralateral occlusion did not show any increased risk compared to patients without this complication,” Krawisz noted.
For the study, the researchers analyzed data from the US National Cardiovascular Data Registry Carotid Artery Revascularization and Endarterectomy (NCDR CARE) registry and the Peripheral Vascular Intervention (PVI) registry. They report that the data represent more than 200 sites, with near equal contribution of stenting and surgery procedures, and include procedures from a diversity of clinical specialties.
All patients who underwent carotid surgery or stenting from 2007 to 2019 in the two registries were included in the analysis.
Results showed that among 58,423 patients who underwent carotid revascularization, 7.9% had a contralateral carotid occlusion. Of those, 69% underwent stenting, and 31% underwent surgery.
The primary outcome was a composite of in-hospital death, stroke, and MI among patients with and those without contralateral carotid occlusion in the surgery group and, separately, in the stenting group.
Unadjusted composite outcome rates were lower for patients with contralateral occlusion after stenting (2.1%) than after surgery (3.6%).
The authors point out that this is particularly notable, inasmuch as patients with contralateral carotid occlusion who were referred for stenting had considerably more comorbidities than patients with a contralateral carotid occlusion who were referred for surgery. “Despite the greater burden of comorbidities, unadjusted in-hospital event rates were lower among those with a contralateral carotid occlusion who underwent stenting versus surgery,” they write.
After adjustment, contralateral carotid occlusion was associated with a 71% increase in the odds of an adverse outcome after surgery (P < .001), compared with no increase after stenting (adjusted odds ratio: 0.94; P = .64).
“Our results show that contralateral carotid occlusion is still one of the primary predictors of a bad outcome in the surgery group but not in the stent group,” Secemsky concluded.
Editorial Raises Questions
An editorial published alongside the study raises several questions about this new analysis.
“This is a well-written paper that adds to the debate on use of carotid endarterectomy surgery and carotid artery stenting in patients with contralateral carotid occlusion,” Gregory L. Moneta, MD, professor of surgery at Oregon Health and Science University, Portland, Oregon, writes. “However, the data does not provide readers with answers to the most important questions regarding the management of patients with contralateral occlusion: who is best managed medically, under what circumstances is carotid endarterectomy or carotid artery stenting best, and what are long-term outcomes?”
Problems with the study that were highlighted by Moneta include the lack of information on outcomes of medical management of patients with contralateral carotid occlusion, and a short follow-up, “likely no more than 1 to 3 days for most patients.”
Secemsky and Krawisz responded in an email to Medscape Medical News: “Medical management has certainly improved dramatically over the last decade, and it will be important to understand outcomes in patients on contemporary medical therapy. Our study provides insight into the management of patients already selected for revascularization, and captures in-hospital event rates which likely account for the bulk of procedure-related events.”
Moneta points out that this latest analysis represents a small subset of a tiny fraction of carotid interventions, which “does not likely reflect national data,” and “like all registries, selection and participation bias within institutions, regionally and nationally, are huge potential problems.”
He adds that confounding is also a problem: “It is entirely likely that those performing carotid endarterectomy and carotid artery stenting differ among themselves in judgment, skill, and performance under difficult circumstances.”
Secemsky and Krawisz argue that the data came from national quality improvement registries with near equal contribution of both stenting and surgery procedures and are widely representative across clinical specialties. They point out that although operator experience always affects outcomes, “given the large number of procedures, the high number of hospitals, and the variety of subspecialties and types of hospitals represented, we likely have reasonable representation of the spectrum of operator skill levels reflective of the spectrum of skill levels patients are seeing in the real world.”
On Moneta’s point that because the study did not compare patients with contralateral carotid occlusion who underwent surgery directly with those who underwent stenting and so “does not inform clinicians seeking patient management guidance,” Secemsky and Krawisz reply that they chose not to do this because the characteristics of patients referred for the two procedures differ substantially.
“Those referred for stenting have significantly more comorbidities than those referred for surgery, and statistical methods are unable to overcome such major differences in populations, as both measured and unmeasured confounders exist,” they note.
The authors write that important conclusions regarding patient management can be drawn from their study.
“Our study showed that contralateral carotid occlusion continues to be a high-risk feature for patients undergoing carotid endarterectomy surgery in contemporary practice and should be a factor used to triage patients to the most appropriate revascularization procedure,” they state.
The study was funded by the American College of Cardiology’s National Cardiovascular Data Registry. Secemsky has served as a consultant and/or on the scientific advisory board of Abbott Vascular, Becton Dickinson, Boston Scientific, Cook, CSI, Janssen, Medtronic, and Philips and has received research grants from AstraZeneca, BD, Boston Scientific, Cook, CSI, Medtronic, and Philips. Krawisz and Moneta have disclosed no relevant financial relationships.
J Am Coll Cardiol. Published online February 15. Abstract, Editorial
For more Medscape Neurology news, join us on Facebook and Twitter.
Source: Read Full Article

