Big change from small player—mitochondrial background modulates whole body metabolism and gene expression
About 1.5 billion years ago, tiny visitors came to live inside the cells that later evolved into all plant and animal life—including humans.
Those visitors were mitochondria, small organelles whose prominent role is producing 90 percent of the chemical energy cells need to survive. Evolutionarily speaking, humans, animals and plants are thus a combination of two organisms.
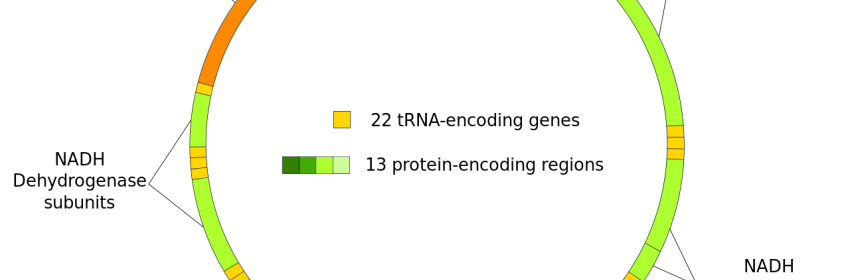
Mitochondria have their own DNA, but the 13 genes in human mitochondria—along with DNA sequences for tRNAs, rRNAs and some small peptides—are massively overshadowed by the 20,000 genes in the human nucleus. Nevertheless, these diminutive mitochondria may have a strong influence on cellular metabolism and susceptibility to metabolic diseases like heart failure or obesity, according to preliminary research by Scott Ballinger, Ph.D., professor of pathology at the University of Alabama at Birmingham.
“For 50 years, researchers have tried to find disease susceptibility using Mendelian genetics,” Ballinger said, speaking about studies of the chromosomal genes in the cell nucleus. “But this explains only 10 percent of the reasons for susceptibility to disease.”
The possible impact of mitochondrial DNA on disease susceptibility depends on two facts. First, all of a person’s mitochondrial DNA comes from the mother, via her egg. This is distinct from the chromosomal genes in the nucleus, where, on average, half come from the mother and half from the father. Second, human mitochondrial DNA has evolved into distinct haplotypes, and each of these types has mitochondrial DNA variations that are inherited together. There are approximately 25 to 35 basic mitochondrial DNA haplogroups, and one of them—found in African populations—has many subtypes due the deep genetic diversity of that continent.
To investigate the impact of mitochondrial DNA, Ballinger and colleagues looked for changes in metabolism and nuclear gene expression when they exchanged mitochondrial backgrounds of strains of mice—specifically those having different mitochondrial DNA sequences, and also having notable differences in susceptibility to diseases associated with metabolism.
After switching the mitochondrial DNA backgrounds, Ballinger and colleagues measured changes in body composition, metabolism and nuclear gene expression in fat tissue when mice switched from a low-fat chow diet to a high-fat diet.
In the first report of its kind, they found that switching the mitochondrial genetic background had a significant impact on adiposity, whole body metabolism and nuclear gene expression in mice.
For example, gene expression in both visceral and subcutaneous fat was markedly changed between mice sharing the same nuclear genome but having different mitochondrial DNA backgrounds, when fed chow versus a high-fat diet. These changes ranged from 10- to 50-fold differences in the number of genes affected, and mitochondrial DNA background influenced whether the number of affected genes were increased or decreased. These studies also found that metabolic efficiency and percentage of body fat in the mice were impacted as well.
Source: Read Full Article